Lost in Transition
Investigation into whether the Ministry of Children, Community and Social Services and the Ministry of Health are taking adequate steps to address the inappropriate hospitalization of adults with developmental disabilities

Table of contents
Show
Hide
Investigation into whether the Ministry of Children, Community and Social Services and the Ministry of Health are taking adequate steps to address the inappropriate hospitalization of adults with developmental disabilities
Paul Dubé
Ombudsman of Ontario
November 2025
Press conference
Report
Acknowledgement of territory
Ombudsman Ontario acknowledges that the province of Ontario is situated on the lands and territory of more than 130 unique First Nations, each with its own distinct cultures, languages, and histories that predate the existence and boundaries of the province.
We acknowledge the existence of political confederacies on these lands that predate both Canada and Ontario, such as the Three Fires Confederacy and the Haudenosaunee Confederacy, who among themselves have treaties and relationships that make up the dynamic landscape of this province.
We humbly recognize that we have collective responsibilities and obligations within the more than 40 treaties in Ontario, such as Treaty 3, Treaty 9, the Robinson Superior and Huron Treaties and the Williams Treaties.
We recognize that Indigenous peoples who have cared for these lands for millennia have been dispossessed by colonization, and we seek to find ways to remedy both historic and ongoing wrongs.
We are grateful to have travelled and worked in First Nation territories and with Métis and Inuit peoples in Ontario since the inception of the Ombudsman 50 years ago.
Ombudsman Ontario is committed to building respectful relationships with First Nation, Inuit, and Métis people and communities in Ontario through trust and transparency in order to be able to provide more services for a shared better future.
Contributors
Director, Special Ombudsman Response Team
- Domonie Pierre
Lead Investigator
- Yvonne Heggie
Investigators
- Armita Bahador
- Chris McCague
- Emily Ashizawa
- Emily Dutil
- Richard Francis
- Rosie Dear
- Sonia Tran
Early Resolution Officer
- Rosemary Bowden
General Counsel
- Joanna Bull
- Laura Pettigrew
Counsel
- Ethan Radomski
- Iris Graham
Executive Summary
1 In an article published in 1960, journalist and author Pierre Berton described his disturbing findings during a visit to the Huronia Regional Centre in Orillia. The piece was a clarion call for reform of Ontario’s system of institutionalized care for people with developmental disabilities. It ended with the chilling words: “Do not say that you did not know what it was like behind those plaster walls, or underneath those peeling wooden ceilings.”
2 In the decades that followed, society responded with a commitment to deinstitutionalization, recognizing the inherent dignity and rights of people with developmental disabilities. Governments pledged to close institutions and replace them with community-based supports, to allow individuals to live with autonomy and dignity.
3 However, while institutions like Huronia have closed, the reality of fulfilling this promise has been complex. Gaps in suitable housing and services have left many without the support they need, leading to a modern form of institutionalization by default. Today, though we no longer intentionally consign people with developmental disabilities to institutional settings, an overburdened and under-resourced system has resulted in some – particularly those with complex needs – being placed in hospitals or other inappropriate settings due to a lack of viable alternatives.
4 In August 2016, I released Nowhere to Turn, my report on the results of my Office’s investigation into the response by the Ministry of Community and Social Services (as it was then called) to cases of adults with developmental disabilities in crisis situations. I observed that because of limited community supports and services, “with nowhere else to turn, those in crisis can find themselves inappropriately housed in a variety of institutional settings from hospitals to jails.”
5 I issued 60 recommendations to the Ministry to address systemic challenges in the developmental services sector. Five of my recommendations specifically focused on the default institutionalization of adults with developmental disabilities in Ontario’s general hospitals and psychiatric facilities.
6 We closely followed the Ministry’s progress in implementing my recommendations, as we continued to receive complaints. Some system improvements occurred over time, but we continued to hear from family members and concerned professionals about the inappropriate and sometimes years-long hospitalization of adults with developmental disabilities. We heard that hospitals frequently managed some individuals by applying chemical and physical restraints, and that the condition of many deteriorated during their long stays in hospitals.
7 When people with developmental disabilities languish in hospital, systemic challenges in the health care and developmental services sectors intersect. By March 2023, I decided to launch a new investigation focused on what is now called the Ministry of Children, Community and Social Services (the MCCSS), as well as the Ministry of Health (the MOH), to determine whether they were taking adequate steps to ensure that such individuals can transition to appropriate homes and supports in the community.
8 This report features the stories of seven people[1] experiencing prolonged and unnecessary hospitalization – waiting months and even years for suitable living and support options:
- Jordan, 25, was in hospital for 15 months, scared and sometimes restrained in a noisy and unpredictable environment.
- Jack, 57, lived in hospital for more than eight years, only to finally move to a home three months before his death.
- Luc, 30, a Franco-Ontarian, was hospitalized for more than four years, often without access to care and services in French, and was regularly subjected to mechanical and chemical restraints. He moved to the community briefly, but returned to hospital, where he remains to this day.
- Noah, 22, was tied to his bed and chemically sedated for most of his more than two years in hospital.
- Sean, 27, lived in a forensic psychiatric hospital for five years, physically restrained at times for up to 20 hours a day, before he transitioned to a supportive living home.
- Kevin, 27, was in hospital, sometimes restrained or isolated, for more than two years before he moved to a community home.
- Anne, 59, desperately wanted out of hospital, but wasn’t able to leave for more than two years.
9 All of them suffered some form of regression, loss of previous life skills, or deterioration in their physical and mental functioning during their time in hospital. Their declining conditions further compromised their ability to find a community home and a willing service agency capable of meeting their needs.
10 As Ombudsman, I have a responsibility to bring “the lamp of scrutiny to otherwise dark places, even over the resistance of those who would draw the blinds.”[2] In this report, as Pierre Berton did in his own way 65 years ago, I have opened the blinds and revealed glimpses into the lives of seven particularly vulnerable people whose personal dignity, integrity, freedom, and quality of life were compromised in an institutional environment that was never designed to meet their needs.
11 Unfortunately, their stories are not unique. They are representative of a broader problem, as evidenced by the multiple complaints we have received about people in similar situations. We know that there are others in Ontario who remain confined to hospital beds, waiting for a home in the community. There is no comprehensive accurate count of the number of people with developmental disabilities inappropriately living in Ontario’s hospitals, the number of people waiting for supportive living, average wait times for that housing, or the number who are served each year. The figures that are available are inconsistent and not generally available to the public. MCCSS documents show there are close to 30,000 Ontarians with disabilities registered for Ministry-funded supportive living. Ministry of Health records suggest that dozens may be waiting in hospital to transition to homes in the community, but the available data from an October 2024 study by the Institute for Clinical Evaluative Sciences and the Centre for Addiction and Mental Health[3] suggest that the number may actually be in the hundreds.
12 I am making 24 recommendations to improve the availability and transparency of supports and services to people with developmental disabilities and complex care needs. I am calling on both ministries to bridge the divide between the health and developmental services sectors, work jointly towards integrated solutions, and undertake proactive system planning to reduce inappropriate hospitalizations in future.
13 This investigation has also confirmed that important recommendations from my 2016 report, Nowhere to Turn, remain unfulfilled. I am hopeful that this new report will serve as a catalyst for both ministries to unite to work toward resolving these systemic issues. I will monitor their progress closely.
Investigation Process
14 This investigation focused on the experiences of individuals with developmental disabilities who remained hospitalized for extended periods while awaiting appropriate housing and support services that would enable them to live safely in the community. We explored the barriers that prevent timely transitions out of hospital, as well as the steps being taken by relevant ministries to address these issues.
15 Between April 2020 and the March 27, 2023 launch of this investigation, we received 15 complaints about individuals with developmental disabilities languishing in hospitals, sometimes for years, with no end in sight. Since the launch of this investigation, we received more than 40 additional complaints about people in similarly difficult situations. In this report, we highlight seven representative cases that illustrate the complex challenges and human struggles they face.
16 Over the course of this investigation, we interviewed more than 120 people, including hospitalized individuals, their family members, hospital and clinical staff, service agencies, Developmental Services Ontario staff, and representatives from community and advocacy organizations. We also spoke with frontline and senior officials from the Ministries of Health and Children, Community and Social Services, as well as Ontario Health. In addition, we reviewed thousands of documents from the ministries and interviewees, and conducted supplementary research.
17 We continue to review individual complaints and make inquiries with government officials, working to resolve the issues wherever possible. Unfortunately, this often proves difficult because of the systemic barriers described in this report.
Legislation Overview
18 For more than a century, Ontario operated segregated institutions to house people with developmental disabilities.[4], [5] During the 1970s, the model for delivering these services began to transition from medical and institutional to community-based programming. In 1974, the Developmental Services Act[6] became law and established a framework for the creation, funding, and operation of community services for those with developmental disabilities. The responsibility for operating Ontario’s 16 institutions also shifted from the Ministry of Health to the Ministry of Community and Social Services. In 1977, the province launched a plan to increase community supports and decrease reliance on institutional care.
19 Today, the Services and Supports to Promote the Social Inclusion of Persons with Developmental Disabilities Act, 2008[7] governs the provision of these services and supports in Ontario. The Act was intended to modernize developmental services, enable more independence and choice, and support transition to a community-based model and greater social inclusion. It also aimed to increase fairness and uniformity in eligibility, assessment and access to services, and to simplify the process for accessing supports, services, and funding.
20 The Act provides for “application entities” to act as a single point of access for services and supports within each geographic region of the province. It also contemplates the creation of “funding entities.” However, the provisions for creating funding entities have never come into force.
21 In 2021, the government published an aspirational vision for long-term developmental services reform, called Journey to Belonging: Choice and Inclusion.[8] The document envisions a future where communities, support networks, and government will support individuals with developmental disabilities to be “empowered to make choices and live as independently as possible through services that are person-directed, equitable and sustainable.” The Journey to Belonging vision also emphasizes proactive planning and integrating supports with other sectors.
Developmental Services and Health Care
22 Adults with developmental disabilities may be admitted to hospital for medical reasons. After their acute medical issues are resolved, some remain because their families or service agencies can no longer care for them in the community. Others do not require medical care, but arrive at hospitals because there is simply nowhere else that can provide the services and supports they require.
23 In some cases, hospitals designate these individuals as “alternate level of care” patients – a term for someone who is occupying a hospital bed even though they do not require acute hospital care. Other “long stay” patients with developmental disabilities are not formally classified as alternate level of care but remain in hospital only because there is no appropriate supportive living accommodation for them in the community. As I noted in Nowhere to Turn, the hospital sector has a longstanding concern about such patients diverting finite medical resources.[9]
24 Adults with developmental disabilities who spend prolonged periods in hospital are involved with two distinct systems: Developmental services and health care.
25 I refer to these clusters of programs and services as “systems” throughout this report. However, they do not necessarily display the interconnected, strategically planned, and organized structure typically characterizing “systems” when it comes to addressing the needs of individuals with developmental disabilities. Some programs and services are ad hoc, reactive, and vary by location. The level of coordination and communication between developmental services and health care services varies when it comes to supporting individuals with developmental disabilities in transitioning to the community.
System overview
26 When someone with a developmental disability remains in hospital because there is no suitable community option, there is a labyrinth of developmental services and health agencies and processes that may be involved to help connect them to needed supports and housing. Collaboration between these entities, along with adequate funding, is usually necessary to establish a suitable transition plan out of hospital.
27 The Ministry of Children, Community and Social Services (MCCSS) and the Ministry of Health (MOH) each have some responsibility in supporting people with developmental disabilities, but they operate from the perspective of their differing mandates. The MCCSS plans, funds, and oversees the developmental services sector, while the MOH stewards the effective management of health services, including hospitals. Part of the MOH’s role includes ensuring that individuals can access “the right care in the right place.”[10]
28 Adults seeking MCCSS-funded developmental services must apply, be deemed eligible for, and be registered with Developmental Services Ontario (DSO), which is the access point for funded supports and housing. Nine regional DSO offices review applications and eligibility for MCCSS funded services within their regions. DSO offices refer eligible individuals to available services and maintain registries for requested services, such as supportive living accommodation, community participation, and short-term respite relief. MCCSS-funded supportive living options within developmental services include group homes, host family homes, supported independent living, intensive support homes, and specialized accommodation. The level of support, including staffing levels, varies depending on the type of home. Intensive support homes and specialized accommodation generally provide 24-hour staffing support and may have access to clinical supports for those with complex needs or a dual diagnosis (having both a developmental disability and mental health diagnosis).
29 Once registered with DSO, there are often long waits for ministry-funded services and supportive living spaces because the demand far exceeds supply. For this reason, DSO uses an algorithm to prioritize access to funded services based on an individual’s level of risk of adverse outcomes, including risk of homelessness. If someone is deteriorating in hospital or at risk of discharge with nowhere to go, this can affect prioritization for service. Therefore, it is important that their hospitalization is communicated to DSO. DSO may also be able to refer an individual with complex or multiple needs to a case manager or to developmental or behavioural services, to help them while in hospital. Such supports are often critical to facilitating communication between individuals (some of whom may be non-verbal) and hospital staff. They can also help mitigate loss of skills and develop transition plans.
30 If there are no funded services or housing options available to meet a person’s needs, as is often the case, DSO may refer their case to a community planning table. Table participants include MCCSS-funded service agencies and sometimes MCCSS representatives, and potentially other sector partners, such as health professionals.
31 Service agencies at the planning table review urgent and priority cases to see if they have appropriate and available resources, including supportive living space or other supports. Agencies have discretion on whether or not to support an individual. They may do so on their own or in collaboration with other agencies and services. For those who have high support and complex care needs, the Community Network of Specialized Care may work with individuals, agencies and planning tables to help coordinate support across service systems, including developmental and health systems.
32 Even if a supportive living space is available, additional funding is often needed to pay for physical modifications and other supports that enable individuals with developmental disabilities to live safely and successfully in the community. Ontario Disability Support Program (ODSP)[11] funding or Passport funding[12] that individuals with developmental disabilities may be eligible for is not intended for purchasing or renovating housing and is often insufficient to cover the costs of hiring direct support staff for those who need full-time support and higher support ratios. These costs can run into hundreds of thousands of dollars or even more than $1 million per year for those with particularly high needs.
33 The MCCSS provides limited funding to build additional capacity in developmental services. Through the Multi-Year Supportive Living program, funding may be allotted annually to support certain prioritized individuals within each region. The funding often helps people who are in inappropriate settings, such as hospitals or shelters, to pay for needed housing and other required services so they can live safely within the community.
34 In addition to the Multi-Year Supportive Living program funding, from 2021 to 2023, the MCCSS and MOH jointly funded a project to help individuals with a dual diagnosis transition out of hospital. Called the Dual Diagnosis Alternate Level of Care Project, it involved collaboration between the ministries, Ontario Health, and MCCSS regional offices. The funding was limited and depended on individuals being identified for consideration and highly prioritized for service. It was also restricted to those with a developmental disability and formally diagnosed mental health disorder (dual diagnosis).
35 In some cases, hospital social workers or a case manager can help connect a person to a private supportive housing option if the individual can afford it or can access government funding to cover the costs. Others may consider an MOH-funded supportive living home if there is one available that meets their needs, though these homes often have long wait times or are not suited to people with developmental disabilities and complex needs.
36 Some individuals may also require clinical supports to transition from hospital to the community, such as psychiatric or nursing supports. Others may need specialized treatment, such as through a hospital-based dual diagnosis program to address behavioural challenges on a time-limited basis. Case managers, complex case coordinators, or hospital staff may be involved to help individuals or service agencies access these services.
37 Ontario Health is a Crown Agency that aims to “connect, coordinate, and modernize” the healthcare system.[13] Its objectives include promoting “health service integration to enable appropriate, coordinated and effective health service delivery”.[14] Ontario Health explained that, as part of this role, they oversee the management of all populations in hospital who require an alternate level of care, which can include individuals with developmental disabilities. Hospitals are responsible for reporting alternate level of care patients to Ontario Health, as the number of hospital beds occupied by people who no longer require hospital care affects access to timely health care for others waiting for a bed. Among the things hospitals can report to Ontario Health is whether someone in an alternate level of care bed has “developmental requirements”[15] that are preventing discharge. Unfortunately, as our investigation found, the numbers are not always reliable.
Suspended Lives: Stories from Hospital Beds
38 The stories of the seven people highlighted in this report illustrate the hardships often faced by adults with developmental disabilities, particularly those with complex needs, when they find themselves stranded in hospitals with nowhere to go.
39 The cases we document include periods of hospitalization during the COVID-19 pandemic. While in some cases the pandemic exacerbated conditions that prevented timely transition out of hospital, it does not fully explain the delays. The systemic barriers that lead to inappropriate hospitalizations and the inability to access suitable services and supportive living existed long before the pandemic and persisted after its end.
40 These seven individuals are not alone. We continue to hear from concerned families and professionals about others in similar situations. As of December 2024, Ontario Health reported that there were 124 adults with developmental disabilities residing in hospitals who no longer required acute medical care. The list is not complete. Hospitals do not always recognize and report that a patient has a developmental disability, and there are various reasons why a hospital might not designate someone as alternate level of care, even though they remain in hospital only because there is no suitable alternative.
41 The stories that follow detail how seven particularly vulnerable members of our society needlessly languished in hospitals, interminably waiting to find a place in their communities. No matter how compassionate and caring staff within a hospital may be, a hospital is not a home.
Catch-22: Jordan’s story
42 Jordan, a 25-year-old who enjoys spending time with his family, spent 15 months in hospital waiting for an appropriate home in the community. He has autism, cerebral palsy, obsessive-compulsive behaviours, and conditions that affect his heart and liver. Jordan is non-verbal and uses a tablet to help him communicate. He also requires help with daily tasks like using the toilet, bathing, and brushing his teeth. Although he had been a happy young man, Jordan’s behaviour deteriorated during the COVID-19 pandemic. He became so aggressive and violent, it was not safe for him to remain at home.
43 As the outbursts escalated at home, Jordan’s mother could no longer work. She told us she grew so hopeless, she thought at one point that the only way to give her husband and other son their lives back might be to kill Jordan and herself. Without sufficient support, she felt “there was no solution...there was no help. There was no end in sight.” When Jordan tried to strangle his aunt while his mom ran an errand, the family was forced to call 911 for help and Jordan was admitted to hospital.
44 In the hospital’s psychiatric intensive care unit, Jordan was scared and often aggravated by the screaming of other patients in crisis. When first admitted, Jordan did not have access to developmental support staff and, without consistent access to his tablet, his parents said he struggled to communicate with hospital staff about his basic needs. At times, he was left to lie in urine-soaked sheets.
45 The hospital told us that staffing ratios did not allow for Jordan to receive the level of care he needed. They also agreed that the psychiatric intensive care unit was an extremely challenging environment for individuals like Jordan on the autism spectrum. There are no routines, and nursing staff frequently change and are not typically trained to communicate with someone with autism. Ill-equipped to deal with his behaviour, hospital staff initially physically or chemically restrained Jordan, sedating him or tying him to the bed. Jordan’s parents said that at times, they needed to be at the hospital up to 12 hours a day to help meet his care needs.
46 Jordan’s mother said they felt trapped in a “never-ending sort of loop.” She said service agencies seemed unwilling to work with Jordan because he was “too violent,” while private treatment programs that could potentially help to address aggressive behaviours turned him down because he would not have a place to live when the program ended. Jordan was in a classic Catch-22 situation: Without treatment, he could not get housing, and without housing, he could not get treatment.
47 Even though Jordan was a high priority for developmental services, no housing vacancies met his needs and there was insufficient Ministry funding for the 2:1 staffing ratio he required. A space for Jordan in the community only opened up when a resident died and Jordan was selected to receive funding through the Ministries’ joint Dual Diagnosis Alternate Level of Care Project. He finally moved into his new home on November 7, 2023 – 15 months after he was first admitted to hospital. Jordan is now doing “fantastically” in his home and sees his parents and brother regularly.
“Get me out of here”: Jack’s story
48 Jack grew up in the community with his family and loved everything to do with cars. He was diagnosed with treatment-resistant schizophrenia, had trouble in school, and never learned to read. However, for five decades, no one identified him as a person with a developmental disability, and he never received associated supports or services.
49 Jack lived in a series of unsuitable housing arrangements throughout his adult life. When not monitored closely, he would drink so much fluid that he would at times have seizures that resulted in hospitalizations. Eventually, unable to care for himself in the community, and with nowhere else to go, Jack ended up spending more than eight years in hospital. He told us he didn’t belong in the hospital and felt like no one was helping him.
50 He also expressed frustration with having no control over his daily activities, including such basic things as when to have a shower. He was concerned about other patients entering his room, and hospital staff said he was assaulted several times by other patients. Hospital staff likened Jack’s living situation during COVID-19 to being in “a jail,” with no access to family or the outdoors beyond the courtyard. During that time, hospital staff said Jack told them he felt like he “didn’t belong anywhere.” They said he pleaded with his mother to “get me out of here.”
51 Only with the support of a persistent and caring hospital staff member was Jack’s developmental disability formally diagnosed. In 2020, he applied for and was deemed eligible for developmental services. It still took another 3.5 years to find a home and suitable funding for him to live outside hospital, as he required 24-hour supervision and a custom-built living space to allow him to live safely.
52 Jack was initially overlooked for the joint Dual Diagnosis Alternate Level of Care Project funding even though he had a dual diagnosis, had been in hospital for years, and was designated alternate level of care. He was only added to the list after our Office made inquiries about his case. Ministry staff said he was likely overlooked because he was in a cognitive care bed in hospital rather than a mental health bed. Eventually, when a resident of a local MCCSS-funded home died and Jack was granted project funding, he was finally able to leave hospital. Tragically, Jack only enjoyed his freedom for three months before he died. He was 57.
Losing hope: Luc's story
53 Luc, 30, is a Francophone who loves computers and is described as a “nice guy.” He lives with severe autism, an intellectual delay, seizure disorder, and obsessive-compulsive disorder. Luc also has a condition that causes him to compulsively and repeatedly pull off his own nails and pick his skin to the point of injury.
54 Even with intensive supports in place, Luc feels compelled to destroy things around him if he sees an imperfection or something that doesn’t match. In a persistent state of crisis and burnout, his family wrote to the MCCSS in February 2020 to seek more help, explaining that the situation at home had become “dangerous.” Sadly, a few days after writing this letter, Luc's family had to call 911 after Luc lost control, started pulling out his fingernails, and head-butted his father in the family car. Luc was admitted to a hospital’s psychiatric unit and, apart from a brief move to a home in 2024, has remained there for close to five years.
55 The hospital’s loud and often tense environment is challenging for Luc. He is confined to his hospital room for long periods. When he becomes agitated, hospital staff use physical restraints or administer medication to sedate him, as they do not have the staff ratios to provide the support he requires. At times, French-speaking hospital staff are not available, which his family and others say results in Luc feeling misunderstood, further contributing to frustration, escalation, and the use of restraints.
56 Extraordinary efforts were taken to connect Luc to supports in the hospital and to find appropriate housing and support for him in the community. A Francophone agency started planning for Luc to transition out of hospital, but this fell through when they realized that Luc’s needs exceeded the support they could provide. Ministry officials worked with a case manager to assess all potential French-language options in the Region. When that proved fruitless, they expanded the search to English-speaking agencies who could provide bilingual services, and even looked out of province. However, service agencies either lacked the staffing and resources Luc required or were reluctant to support someone who had only lived at home or in the hospital when pandemic related visitor restrictions prevented them from meeting with him in person to assess current skills and behaviours. During the search, regional staff documented that “[t]here is a clear lack of current capacity to provide high support residential care in the… area to individuals with extraordinary behaviour needs….”
57 Finally, after more than four years in hospital, an agency agreed to transition Luc to the community, but his respite was short-lived. After only six months, the agency could no longer manage his behaviours. Despite 3:1 staffing, psychiatric support, and the services of a behavioural therapist, several staff were injured. Luc was again admitted to hospital, and shortly thereafter, the agency providing behavioural support withdrew its services. He was essentially back to square one. After several months in hospital, another service agency offered to potentially develop a support plan to enable Luc to transition out of hospital. These efforts are ongoing, but, in the meantime, the family is again concerned that he is being restrained in his hospital bed for long periods, rarely able to leave the psychiatric unit, and losing hope.
“Quite inhumane”: Noah’s story
58 At 22, Noah is described as “full of life” and enjoys listening to music and going for walks. He is on the autism spectrum, non-verbal, suffers from anxiety and seizures, and functions developmentally as a 12-18-month-old. Raised at home by his mother, Noah never attended school and had limited involvement with developmental services. As he got older, Noah’s behaviour became increasingly aggressive and difficult to manage. His mom repeatedly feared for his and her own safety and either brought Noah to hospital or called emergency services. After a series of hospital admissions and discharges, Noah was admitted to hospital in August 2021 and remained there for almost two and half years.
59 In his first few months of hospitalization, those supporting him said that he was relatively “restraint free.” However, by his eighth month in hospital, his self-injurious and aggressive behaviours were escalating. Noah was tethered to his bed through all of his waking hours, in a spreadeagle position using either three or four-point restraints. Hospital staff also regularly chemically restrained him with sedating medication. Those close to Noah told us that he went from being able to toilet, bathe, and dress with limited help to using a diaper, needing assistance to walk, and losing his basic life skills. When staff were unavailable to take him to the washroom or change his diaper, Noah lay in his own urine-soaked bed sheets, sometimes for hours.
60 During his last year in hospital, Noah’s diapers became so saturated that they would form chunks, which Noah began to pick at and eat the pieces. A professional working with Noah documented that he spent “no longer than 60-120 minutes per day out of restraints.” Noah’s mother told us he would bang his head on his bed while he was tied down – and twice injured himself to the point of bleeding. He also frequently kicked the wall and injured a toe so severely that it had to be amputated.
61 A professional supporting Noah who observed him in hospital remarked, “You feel completely like...you’re witnessing almost...a profound level of neglect that you can’t do anything about…” Another said that this was “the worst case I’ve ever been involved in and ...it has a profound impact on the people that support him...I would like to know if there’s anybody in Canada who’s being treated as poorly….”
62 The extensive use of restraints, we were told, largely frustrated efforts to assist Noah. One clinician explained that they were unable to get Noah to a “community-ready state” in a hospital environment under these conditions. By summer 2022, DSO classified his needs as having increased to the maximum level. DSO staff said they had never seen this before and it was likely due to the extended use of restraints, increased aggressive behaviours, seizures, and mobility issues acquired during his stay in hospital.
63 Despite being near the top of the priority list for developmental services, it proved difficult to find suitable housing and support for Noah in the community. His profile was considered through the local planning table’s urgent response process, and added to registries outside his immediate area, but no service agency initially came forward to help him. In an effort to encourage agencies to step forward, Noah’s case manager updated his service profile to better reflect his personality and interests before he entered the hospital. She also emailed the Ministry, saying “things are getting quite inhumane” in hospital, and asking to meet to discuss a plan for Noah.
64 Finally, in December 2022, after MCCSS regional staff organized a meeting bringing together the case manager, Ministry-funded service agencies, and the Community Network of Specialized Care, a service agency came forward and began to plan for Noah to transition to the community. After months of searching, the agency located a single-family home it could rent for Noah – if it received sufficient capital funding to make the space suitable for his needs and additional funding for 2:1 staffing support. The agency confirmed Noah met the criteria for Dual Diagnosis Alternate Level of Care Project funding and, in October 2023, the Ministry approved an annual budget for him. In March 2024, he moved into his new home. Service agency staff now support Noah in the home, with local hospitals providing needed psychiatric and behavioural therapy. After two years largely confined to his hospital bed, Noah now wears his own clothes, no longer requires a diaper, and can even play soccer in his yard.
Unfit to stand trial: Sean’s story
65 Sean enjoys playing basketball, video games and listening to music. He is 27, but functions at approximately the cognitive age of a 5-year-old. He has been diagnosed with autism and chronic adjustment disorder, and lives with a stoma as a result of a Crohn’s disease-related colostomy surgery he had as a teenager.
66 Sean has aggressive behaviours and can become violent. By January 2019, his family was frequently calling police for help. One record we reviewed noted the family had called emergency services 28 times in the span of eight months; another documented more than 20 short-term visits to six different hospitals within seven months. Psychiatric specialists consulted on Sean’s case recommended more community-based supports and behavioural interventions. They observed that hospital environments exacerbated Sean’s behaviours and recommended solutions outside of hospital settings.
67 At home, the family continued in a state of crisis. Recognizing that the situation was not sustainable, service agencies made efforts to connect Sean to additional support and added him to a waitlist for a specialized treatment bed to provide short-term intensive treatment to help stabilize his behaviours. They wrote that without a safe and secure housing option with access to behavioural supports for Sean, “an extremely unsafe, untenable and dangerous situation and harm” would continue.
68 Unfortunately, no option was found, and Sean attacked his mother at home in December 2019. This time police suggested he be charged criminally to compel necessary supports through the justice system. After police laid charges, the court issued a no-contact order preventing Sean from returning home, and he was admitted to hospital under the Mental Health Act. The court later found Sean “unfit to stand trial” and remanded him to a psychiatric treatment hospital. The Ontario Review Board ordered that he remain there until housing with 24-hour supervision in the community could be located.
69 However, with no appropriate housing and services available to meet his needs, Sean remained at the psychiatric hospital for more than five years.
70 To manage Sean’s aggressive behaviour and self-harm, the hospital relied on mechanical restraints at various points during his hospitalization, at times up to 16-20 hours a day. Developmental sector staff supporting Sean observed that the transition from living with his family to a secluded hospital setting was scary for Sean, and behaviours were exacerbated by the frequent staff turnover because he does not do well with change and struggles with new people. While Sean had previously been able to participate in the care for his stoma, his self-injurious and aggressive behaviours increased in hospital and the process now took six staff to complete.
71 Efforts to find Sean a home were further complicated by his aggressive behaviours and complex medical needs and, at times, he was not medically cleared for discharge. His needs increased because of the time spent in hospital, which meant he would require a higher staffing ratio in the community than he would have before his hospital stay, at a much higher cost. A rural location was initially considered but ruled out primarily because of the distance from medical supports, the complexity of transporting Sean long distances to receive care, and the service agency’s inability to recruit sufficient staff in the area.
72 Finally, when a supportive living vacancy located in a city arose, the service agency supporting Sean was able to renovate that space and arrange necessary staffing and supports with sufficient Ministry funding and access to nursing and psychiatric support. Since moving into the home, Sean is now able to go outside, celebrate holidays, and live more independently. A sign Sean made for his entryway reads, “This is my forever home.”
Worse than prison: Kevin’s story
73 Kevin, 27, loves listening to music. He has autism, is largely non-verbal, and lashes out aggressively when he’s frustrated. His mother told us she felt unsafe every day when Kevin lived at home with the family. She worried about Kevin’s younger brother, who would hide in his room to feel safe. Kevin was registered in a day program and the family was able to obtain some services with Passport funding but, when his supports fell away due to the pandemic and other issues, the situation at home escalated.
74 The family was registered for supportive living through DSO but were told it could take years to access housing, even though Kevin was a priority in the community.
75 Kevin’s parents struggled to manage his behaviours at home. Police were called on multiple occasions in response to his violent behaviour, which would lead to him being taken to hospital and then discharged. At one point, Kevin bit his father’s finger so badly that it required surgery. In November 2020, after another episode of aggression, police were called, and Kevin was brought to hospital and ultimately admitted to the psychiatric unit.
76 His mother described the hospital setting as “worse than prison.” To manage his behaviour, Kevin was monitored by security guards, sometimes restrained or isolated, and had few opportunities to leave his small unit. Hospital staff acknowledged that the psychiatric unit was not the best environment for Kevin. His physical and mental health declined, and he seldom smiled like he used to. Despite the hospital being “desperate to discharge” him and local planning tables identifying him as “one of the highest need [individuals] for high behavior [supportive living],” it took more than two years to transition Kevin to a home outside hospital.
77 Initially, there were no suitable vacancies for Kevin and the Ministry did not know what, if any, funding would be available to support him.
78 When he was diagnosed with a mental health condition after a year in hospital, he was one of a select few individuals who qualified for Dual Diagnosis Alternate Level of Care Project funding. However, he still had to wait months for another resident to move out of existing housing before an appropriate spot opened for him. Kevin finally moved into a home with a yard in January 2023.
“I just give up”: Anne’s story
79 Anne loves knitting, swimming and animals. She has autism, generalized anxiety disorder, a mild developmental delay, and struggles with obesity. She is 59, but wasn’t connected to developmental services until she was over 50 – and has experienced several living arrangements that broke down or did not meet her needs.
80 While living in a supported independent living home that did not provide the level of support she required, Anne was intermittently admitted and discharged from hospital. Finally, desperate for a change and believing that someone would come and get her, Anne left her supported independent living home to go to a hotel. She was found by hotel staff three days later, alone and unable to get up, lying on a soiled bed with nothing to drink and only dry cereal to eat. They called an ambulance.
81 Anne was re-admitted to hospital in late December 2020 and, a few months later, transferred to a specialized dual diagnosis program in another hospital. She returned to the local hospital in May 2022 and remained there for two and a half years. Anne told us that she spent most of her time in hospital in bed, and she wanted to live on her own in the community where she could have friends. She said she felt stuck and said of the lengthy hospital stay, “I just give up because... I’m not happy.”
82 Hospital staff, DSO, and a complex case manager with the Community Network of Specialized Care all worked to find housing options for Anne, but she was passed over for seven funded spaces because her needs “didn’t quite match.” Ministry staff said they believed Anne’s mental health needs, along with a lack of funding, were a barrier to finding a suitable home. After more than two years in hospital, Anne was not considered for Multi-Year Supportive Living funding and was overlooked for Dual Diagnosis Alternate Level of Care funding – until our Office made inquiries into her case. Hospital staff who were trying to help her find a home expressed frustration and concern about how Anne was being treated. They noted that it was neither patient-centred nor an appropriate allocation of resources, given that she was in a publicly funded acute care bed.
83 Two options with private service agencies arose while Anne was hospitalized, but they fell through. Even though Anne had been rejected for several Ministry-funded housing options, the Ministry told us that private agencies are only considered as a last resort, and there was just no funding available. Anne was also added to the waitlist for a MOH supportive living home, but after a year had only moved from 11th to eighth position on the list.
84 Finally, Anne was able to move into a private retirement home for seniors after a service agency involved in her case agreed to pay the upfront costs from its operating budget, with Ministry reimbursement in the new fiscal year. Despite the financial hardship it faced, the service agency agreed, just to help get Anne out of hospital. Three days after the transition, the agency told us she was doing remarkably well, and they were seeing the “best version” of her. After four months living in the retirement home, her case manager said Anne was continuing to do well, was regularly eating with other residents in the dining room and had been able to visit with her previously estranged daughter.
High Demand, Short Supply: Barriers to Transition
85 The primary reason for prolonged hospital stays is the chronic shortage of suitable supportive living accommodations in Ontario. There was no acute medical need for the seven people featured in this report to remain in hospital, but there was nowhere for them to live safely in the community.
86 For years, the demand for supportive living accommodations in the developmental services sector has far outstripped supply. Between 2020 and 2024, the number of people registered with DSO who were waiting for supportive living increased from almost 24,000 to 28,500.
87 An internal briefing note to the Minister of Children, Community and Social Services in April 2023 noted that this number had grown at an average rate of 9% per year over the previous four years, with “essentially” no increases in the number of people served.[16] Indeed, the provincial Financial Accountability Office’s 2024 review of Ministry spending found there was a general trend of “no growth” in the number of clients served in supportive living since 2017-2018, and that this had contributed to the growing waitlist. The Financial Accountability Office reported that the number of people waiting for supportive living increased 49% between 2017-2018 and 2022-2023.[17]
88 Because of limited vacancies, DSO uses an algorithm to prioritize individuals for service, based on the associated level of risk to health or safety. A person’s risk level depends on their current living situation and their behavioural, personal, and medical support needs, as well as their caregiver’s circumstances. When a vacancy arises within MCCSS-funded supportive housing, DSO will first consider those with the highest priority scores for the vacancy.
89 A Matching and Linking Coordinator reviews the prioritized profiles to assess the best “match,” considering such factors as personal preferences, compatibility with any other residents in the home, and whether there are sufficient staffing levels to meet the person’s needs. However, DSO told us those with more complex needs often cannot be matched to existing funded vacancies. As one official in developmental services observed, Luc is “a perfect example of someone that cannot be matched within our group homes because he requires too much support.”
90 Some MOH-funded supportive housing, which is intended for individuals with serious mental illness or addictions, can also serve individuals with a dual diagnosis in certain circumstances. Demand for this housing also exceeds supply, although there is no standardized information about wait times. In 2016, Ontario’s Auditor General recommended that the Ministry regularly collect waitlist and wait time information by region.[18] Despite this recommendation, at the time of writing this report, the MOH still did not track wait times for supportive housing.
91 In the absence of provincially consolidated information about wait times, evidence suggests that individuals can face lengthy waits. A February 2024 report by the non-profit agency Addictions and Mental Health Ontario described multi-year waitlists for MOH supportive housing. That report notes that those with serious mental illness and complex needs who require 24-hour high support housing in Toronto, for example, may have to wait up to five years.[19] A March 2025 follow-up report by the same organization said waitlists were “at crisis levels.” They estimated that the average wait time for mental health supportive housing in Ontario was nearly four years, while in Toronto the average wait exceeded eight years.[20] The report also documents a growing need for high-support housing units, with a Toronto housing coordination agency reporting that 40% of applicants who were declined had needs that exceeded available service. It states that many of those waiting may be in shelters, hospitalized, or in housing that does not meet their needs.
Turned down and passed over
92 When DSO is unable to match people in urgent need to available MCCSS-funded vacancies, it refers them to a community planning table, and sometimes community tables in other jurisdictions, where ministry-funded service agencies in the area try to find or develop a solution. One senior official at an agency that helps connect families to available services said this referral was typically a “formality” rather than a solution for individuals like Luc or Noah, because agencies that are willing or able to support individuals with extensive complex needs are so scarce. A hospital’s Dual Diagnosis Coordinator in another region said that they have never had a long-stay patient with a developmental disability go into an existing funded supportive housing arrangement.
93 Individuals with the highest needs may instead have to rely on private agencies for supportive housing options. However, private agencies also struggle to provide the required capacity and resources. In Luc’s case, one private agency considered supporting him, but did not have sufficient staffing resources. Another did not have bilingual staff to provide the French service he requires.
94 Even if a private service agency offers to step in with a supportive housing space, the option may fall through because of lack of funding. In Anne’s case, when the hospital found a private agency willing and able to meet her needs, MCCSS funding was not available and she remained in hospital. Ministry staff in that region told us they would only fund private agencies as a last resort because they would rather build capacity within the funded system. However, by the time planning for Anne’s housing with a private agency collapsed, her case had already been presented to various planning tables throughout the region multiple times – and she’d been rejected for at least seven vacancies. Similarly, Jack’s profile was circulated to community planning tables for years, with no success.
95 These are not isolated cases. Hospital staff we interviewed and Ministry documents we reviewed[21] confirmed that individuals with developmental disabilities have been stuck in hospitals for periods of 10 years or more because no service agencies could be found to support them in the community.
Institutionalized in hospital
96 The longer someone with developmental disabilities remains in hospital, the more challenging it can be for them to transition to the community. Hospital staff told us the longer the hospital stay, the more reliant the person may become on higher staffing ratios and staff doing daily tasks for them. Over time, they acclimatize to hospital routines, and it becomes harder to establish or adapt to new ones. As one MCCSS official put it: “Experience has shown that the environment in which an individual is supported will condition their ability to adapt to living in the community.”
97 One hospital told us about a man in his 30s with an intellectual disability and significant mental health disability who had spent almost 14 years in hospital. They said the hospital determined that the man did not require hospital-level care shortly after he was admitted in 2009. Community planning tables considered his profile monthly for nearly eight years before an agency finally agreed to support his transition to the community. Unfortunately, he returned to hospital soon after, because the agency could not manage his behaviours. Hospital staff told us they believe the man had become “institutionalized” and came to think of the hospital as his home.
98 The loss of independence and life skills can increase the resources needed to support a person who has become institutionalized, making it more challenging for service agencies to plan for and support them in the community. A behavioural consultant who has worked in the sector for more than 20 years told us the people who get stuck in hospital have a “documented profile that can appear quite… difficult to support,” causing agencies to be hesitant to offer services. For example, unlike hospitals, developmental service agencies do not generally have the infrastructure or specialized staff necessary to respond when someone becomes extremely aggressive.
99 One MCCSS official explained that service agencies often “skip over” those with very complex needs – a vicious cycle that makes it more difficult for them to leave hospital as their stay continues.
100 Many of the cases highlighted in this report demonstrate the significant detrimental impact that a lengthy hospitalization can have. After years in hospital, Jack lost independence and increasingly required assistance with simple daily tasks. Noah lost his basic toileting skills and had been restrained in a hospital bed for so long, no one could predict how he would react outside of hospital. A service coordinator commented that “very, very few agencies would ever take somebody coming out of hospital in four-point restraints.” Even when an agency, moved by Noah’s compelling circumstances, finally offered him a home, his transition to the community was only possible with additional funding for renovations and added access to psychiatric and behavioural staff – and it took a further 15 months before everything was in place to allow him to move.
101 Ultimately, service agencies have discretion to determine whether they have capacity to support someone. MCCSS staff acknowledged that some service agencies do not want to assume the risk of someone with high behavioural needs harming staff, and said if a person transitions to a service agency that does not have the capacity to support them, there is a risk of doing more harm. We saw this in Anne’s case when she ended up in a hotel room unable to care for herself after moving into a ministry-funded home that did not meet her level of need. However, Ministry staff also said it is part of their oversight role to make sure agencies are considering more than their liability, as providing services to “vulnerable citizens” is “the bottom line of what [they] do.”
A “maxed out” system
102 Even when a service agency is willing to support someone with very complex needs, there is often just no appropriate space ready for them to move to or that could be converted to meet their needs. One MCCSS official told us that when institutions in the developmental services sector were closing between 1977 and 2009, steps were taken to create capacity to support people with high needs. The sector also created “unfunded capacity,” including an inventory of spare rooms, bedrooms, and other living units that could be used for future expansion. Unfortunately, this practice did not continue – and today, space in the sector is “maxed out.” Homes in the community are either fully occupied or the space is no longer suitable for new individuals to occupy because of changes in requirements like regulations, municipal by-laws, and fire safety codes. One Ministry official expressed concern that developmental services housing is at a “critical point,” as service agencies say there are no more spaces to convert.
103 The decreasing housing supply in the developmental services sector was predicted in an October 2018 Ministry Program Note.[22] It stated that service agencies had been asked to use available housing resources when undertaking multi-year planning to support the highest-priority individuals, “but system capacity will be reduced without additional investment to address rising costs and service demand.”
104 One Ministry official told us that now, “basically somebody has to pass away in order to create a vacancy.” The parents and service providers we spoke with made similar observations. Both Jordan and Jack were only able to leave hospital once a resident in a Ministry-funded home died. One MCCSS statistic from 2019 showed that each year, 1,500 new people request funded supportive accommodation, while only approximately 450 leave these spaces.[23]
105 The MOH does not track demand for its supportive housing programs, some of which we were told could support those with a dual diagnosis. However, a February 2024 report on mental health and addiction supportive housing stated that supportive housing providers were not confident that the system had capacity to support an increasing volume of people with complex mental health needs.[24]
A troubling trend
106 While the lack of appropriate housing is a long-standing issue in the developmental services sector, there are indications that the situation is getting worse. An April 2023 MCCSS Minister’s Briefing reported an 8% increase in the number of individuals with high support and complex support needs over the previous year.[25] It noted that the number of individuals with autism receiving funding through the Ontario Disability Support Program had increased by 5% between 2017 and 2022, with 20% of 18- to 24-year-olds with autism having “exceptional” behavioural needs. Another internal Ministry document from September 2021, related to the Dual Diagnosis Alternate Level of Care Project, estimated that 20% of patients with dual diagnosis at Ontario’s psychiatric hospitals were designated as alternate level of care – and nearly half were waiting for community-based housing with a high level of support.[26]
107 One Ministry official candidly told us that, given the level of complexity and concurrent disorders, “the solutions we’ve been using are no longer meeting the needs of the people coming into the system now.”
108 Parents caring for their adult children with developmental disabilities at home are also aging. The April 2023 MCCSS Minister’s Briefing stated that 11,200 people with developmental disabilities live with a caregiver aged 60 or older, and this was expected to increase to approximately 17,400 over the next five years.[27]
109 It is troubling that the rise in the complexity of care needs and the aging population of caregivers come at a time when there are so few community resources available for those considered hardest to serve. The higher someone’s needs, the fewer resources there are. If these trends persist, inevitably, acutely vulnerable individuals with developmental disabilities will continue to languish in hospitals and other inappropriate settings. As we saw with the people featured in this report, many of those left in hospital will deteriorate mentally and physically and lose valuable life skills, making it harder and often more costly for them to transition to living in the community. At the same time, they will continue to occupy a bed that might be needed by someone in need of acute medical care. Families, hospital staff, and developmental services professionals will keep struggling to find solutions that do not exist, leaving the public to pay the price for a system that delivers the wrong care, in the wrong place.
Still Nowhere to Turn: Systemic Gaps
110 Nine years ago, in my 2016 report, Nowhere to Turn, I addressed the extremely troubling lack of suitable housing options for people with developmental disabilities who demonstrate aggressive or violent behaviours.[28] I also encouraged the Ministry to engage in research and consultation across the developmental services and health sectors. The aim of this was to develop supportive living resources that meet these individuals’ exceptional needs. I recommended that the Ministry create an inventory of suitable housing options, as the system was leaving many improperly housed in hospitals, shelters, long-term care homes, and even in jails.[29] The Ministry did conduct research on supportive living arrangements for individuals with exceptional medical and/or behavioural needs, but an inventory of housing to meet these needs remains lacking.
111 Since 2016, lack of supportive living spaces in the developmental services sector has continued to be a key barrier for those inappropriately housed in hospitals. As the Financial Accountability Office reported in 2024, there has been a trend of “no growth” in the number of people served within developmental services supportive living since 2017-2018.[30] The system remains reactive and fragmented.
Research on repeat
112 The lack of suitable housing options for those with developmental disabilities with complex or co-occurring needs is not a new issue. For more than a decade, researchers have warned about the problem, suggested solutions and called for action.
113 In 2009, the Centre for Addiction and Mental Health published From Hospital to Home: The Transitioning of Alternate Level of Care and Long-stay Mental Health Clients.[31] The report, commissioned by the then-Ministry of Health and Long-Term Care, found that a shortage of high-support housing, combined with “coordination challenges” between the health and developmental services systems, contributed to the hospitalization of people with dual diagnosis as alternate level of care patients. The Centre recommended that the ministries responsible for health and developmental services work together with those responsible for regional administration of public health care services to develop appropriate supportive housing options for people with dual diagnosis. It also encouraged greater communication and collaboration between the community and hospitals before these individuals are discharged, to ensure appropriate supports are in place.
114 In 2012, KPMG issued a report[32] commissioned by six Ontario psychiatric hospitals that assessed the hospital dual diagnosis programs and system gaps for those with dual diagnosis. It found that, amongst the six hospitals, this population accounted for 37% of alternate level of care patients. Participants in the review included physicians from hospital dual diagnosis programs and representatives from the Community Networks of Specialized Care. All identified limited access to supportive housing with adequate staffing levels and skills as a contributing factor to the high number of alternate level of care patients with dual diagnosis in hospitals. The report found there was a need for a broader range of housing, “especially for individuals with higher support requirements for their complex needs.”[33]
115 In 2014, the MCCSS created a Developmental Services Housing Task Force to research innovative solutions to the “severe housing shortage” in the developmental services sector. In 2018, the Task Force made recommendations to the Ministry about researching issues and inter-ministerial solutions to address situations faced by people with developmental disabilities, including those who have multiple needs or who are in complex or precarious housing situations, noting that the current approach was leaving thousands without the housing supports they need.
116 In February 2019, the Health Care Access Research and Developmental Disabilities program at the Centre for Addiction and Mental Health, the Institute for Clinical Evaluative Sciences, and the University of Ontario Institute of Technology released a report entitled Addressing Gaps in the Health Care Services Used by Adults with Developmental Disabilities.[34] They observed that patients with developmental disabilities are 6.5 times more likely to be classified as alternate level of care than others, and that this indicated problems with the availability or accessibility of appropriate community-based supports. The report also found that for those with both a developmental disability and mental health diagnosis, the likelihood and frequency of emergency department visits and hospitalizations increased.
117 In 2022, the Centre for Addiction and Mental Health produced a Housing and Mental Health Policy Framework[35], which noted the particular challenges that alternate level of care patients with serious mental illness and complex needs have to access housing. The Framework includes a recommendation for MCCSS and MOH to work collaboratively to create targeted housing initiatives for individuals with dual diagnosis.
118 In 2023, the Centre for Addiction and Mental Health published a report commissioned by the MOH through the Dual Diagnosis Alternate Level of Care Project, called Supporting Alternate Level of Care Patients with a Dual Diagnosis to Transition from Hospital to Home: Practice Guidance.[36] It echoed previous findings and recommendations, encouraging the health and developmental services sectors (including the two ministries and Ontario Health) to work together to establish and adequately resource a minimum set of core services for individuals with dual diagnosis. It suggested that these standard services should be available and accessible across the province and that there should be a range of housing and community support options with appropriately trained staff. The report also noted that data on population needs should inform decisions about housing models.
Progress hindered
119 Despite these repeated well-founded calls for action and recommendations for reform, negligible progress has been made to increase the availability of adequate supportive living accommodations in the community for people like Jordan, Sean, Jack, Luc, Noah, Anne, and Kevin.
120 In all the cases highlighted in this report, finding an appropriate Ministry-funded service agency or a private agency capable of providing support in the community for individuals with multiple or complex needs was a difficult and often years-long process. This was true even when individuals were identified as a high priority for receiving services in their communities.
121 Numerous officials across the health and developmental services sectors told us they were frustrated about the lack of suitable housing resources for these individuals. Some described the absence of suitable housing as the biggest barrier for those seeking to leave hospital. One hospital employee commented that trying to find a suitable home in the community for someone with a developmental disability, particularly someone with a dual diagnosis, was “virtually impossible.”
122 In Nowhere to Turn, I described hospitals as a Band-Aid solution to the problem of limited housing in the developmental services sector. I observed: “Today’s developmental services system does not reflect long-range strategic planning on the part of the Ministry, but rather a matrix of diverse and individualized visions of hundreds of non-governmental agencies involved in this sector.”[37]
123 After the release of that report, I saw some progress towards system planning to develop both developmental services housing and supportive housing generally. In 2017, the then-Ministry of Community and Social Services and the Ministry of Health collaborated with other ministries to create a cross-sector Ontario Supportive Housing Policy Framework.[38] The framework stated that supportive housing was key to enabling individuals with complex needs “to find stable housing, lead fulfilling lives, and live as independently as possible in their community.” Its stated goals included developing a more coordinated system where ministries, local entities like service managers, Local Health Integration Networks (now part of Ontario Health), housing providers and others worked together toward a more person-driven approach to meeting housing needs.
124 The MCCSS took some steps to address recommendations from Nowhere to Turn, including seeking ways to prioritize those with complex needs and investing in capacity building within the developmental services sector. By April 2018, it had developed a Developmental Services Housing Strategy[39] directed at increasing access to a range of person-centered, affordable housing and support arrangements to meet individuals’ unique needs.
125 That same year, the Ministry had also proposed an initiative intended to expand supportive living options specifically for prioritized individuals inappropriately housed in settings like hospitals, long-term care homes, and correctional facilities. The projected budget was $31 million. Under the initiative, there would have been dedicated resources for inappropriately housed individuals through the Multi-Year Supportive Living Program.
126 However, after a change in government and a government-wide cost-saving directive, the Ministry’s Assistant Deputy Minister of Business Planning and Corporate Services issued a memo to the MCCSS Management Committee asking all program areas to revisit their budget forecasts. Among other things, they were asked to slow down and scale back any spending, and revise program strategies to achieve savings, including by delaying implementation.[40]
127 In response, MCCSS staff prepared an Information Note for the Minister, setting out their expenditure management strategy for approval.[41] The items for which the Ministry would no longer seek funding included $25 million allocated for housing supports and $6 million in capital for inappropriately housed individuals. Other proposed initiatives – such as innovative housing, “living at home longer,” and new supportive living and respite spaces – were also removed from funding consideration.
128 At the same time in 2018, as the Ministry’s plans to seek funding for increased housing resources in the developmental services sector were abandoned, the Developmental Services Housing Task Force that the Ministry had created in 2014 was calling for a solution to the “crisis-driven approach to housing needs” in the sector. In its report, “Generating Ideas and Enabling Action: Addressing the Housing Crisis Confronting Ontario Adults with Developmental Disabilities,”[42] the Task Force emphasized that as housing waiting lists continue to grow, system planning must shift into “prevention” mode. The report assessed and analyzed 18 collaborative and innovative housing projects, some of which supported individuals with complex needs.
129 According to Ministry documents, MCCSS intended to evaluate those models to identify best practices that could be replicated with new investment in innovative housing and to fully leverage other community partnerships to increase the range of available housing. However, by July 2019, an internal Ministry Developmental Services Reform Foundation paper noted that MCCSS still did not have a broad strategy to “effectively and efficiently” reform supportive living services, which it said should include an official developmental services housing vision supported by stakeholders.[43]
Back on the back burner
130 The momentum that followed the release of my Nowhere to Turn report faltered and stalled. Efforts to address the problem continued, but progress has been slow and limited.
131 In 2020, a KPMG review of developmental services submitted to the MCCSS observed that Ontario was underperforming in “marketplace reform.” While the report said high-performing agencies were undertaking innovative initiatives, there was no mechanism to scale those initiatives across the province.[44]
132 That same year, the Central East Local Health Integration Network created a working group to seek more proactive solutions for people with a dual diagnosis who found themselves stuck in hospital. The working group, which included representation from MCCSS, reviewed the profiles of those who remained in hospital because they could not be served within the existing developmental service system. The working group was asked to find solutions that would ensure that individuals with dual diagnosis and high needs were served appropriately.
133 The working group reviewed data and patient profiles over several years. In 2021, they reported that patients in hospital with unmet housing needs often:
- Had developmental delay and multiple, separate mental health diagnoses;
- Were diagnosed on the lowest end of the autism spectrum (typically, non-verbal, or with very limited abilities);
- Required assistance with most aspects of daily living;
- Had elevated behavioural scores; and
- Had a history of aggression and/or criminal justice involvement.
134 The authors noted that the number of individuals within this profile was “relatively small.” The review also noted that the longer the hospital stay, the harder it was to find housing. Its list of key supports needed in the community for long-stay patients with complex needs include multi-organizational specialized clinical support teams, increased specialized housing, dedicated funding for housing renovations, cross-sectoral partnerships between disability and mental health supportive housing providers to ensure integrated supports and services, and a systems planner for housing.
135 Ontario Health officials familiar with the project told us the work done was “fantastic,” but progress stalled because of insufficient resources, staffing challenges, and shifting priorities.
136 In an internal document from 2022[45], MCCSS officials observed that supportive housing could reduce reliance on higher-cost government-funded services, “such as emergency room visits, hospital stays, police interactions, justice system involvement (including jail) and long-term care.” Another internal document from this period acknowledged that current housing capacity was insufficient and made several suggestions for reform. One was to leverage partnerships to increase affordable supportive housing with the proviso: “We can’t do it in silos.”[46]
137 Despite these multiple and extensive studies, there is still no detailed plan aimed at supporting those with developmental disabilities and other complex needs who cannot find suitable housing options. Many of the senior MCCSS staff we interviewed said they were unaware of any existing developmental services supportive living strategy.
138 There have been some efforts to develop a collaborative “Multi-Ministry Supportive Housing Initiative” for supportive housing, led by the Ministry of Municipal Affairs and Housing. But both the MCCSS and MOH described this as being in its “early stages.” The initiative is focused on supportive housing for “vulnerable populations” generally, and it is still unclear whether or how it will help to address the housing gaps for those with the most complex needs.
139 The MOH is also leading policy development for a Local Integrated Supportive Housing requirement under the Multi-Ministry Supportive Housing Initiative. Staff told us a draft policy is being developed and is intended to require health sector partners to work with municipal service managers and developmental services to plan supportive housing, rather than working in silos. This is similar to the multi-sector collaboration requirements in the 2017 Supportive Housing Framework. However, as of early 2025, Ministry of Health officials told us this work was on the “back burner,” as focus had shifted to rolling out Homelessness and Addiction Treatment Recovery Hubs to replace safe drug consumption sites. They said that supportive housing will be part of the hubs and some of that housing may support individuals with a dual diagnosis. However, they observed that it was unlikely to be of assistance for alternate level of care patients with developmental disabilities and complex needs, similar to those described in this report. It is also unlikely to assist those with developmental disabilities who do not have a mental health diagnosis or addiction.
140 Although little progress has occurred at the provincial level on implementing a capacity-building housing strategy for the developmental services sector, we did hear about several local community-specific initiatives aimed at increasing high support service options. For example, a Toronto service agency worked with a local hospital’s outpatient service to build housing capacity for individuals with complex needs, including those with dual diagnosis. The Dual Diagnosis Alternate Level of Care Project funding and other ministry funding assisted several individuals to transition out of hospital to this housing. In the East region, there is a committee of service agencies reviewing how they can collaborate to deliver housing and supports for those with higher support needs. These initiatives are promising, but they do not represent the coordinated and comprehensive approach required to address this problem across the province.
A reactive and insufficient approach to capacity building
141 Without a proactive capacity-building plan for individuals with developmental disabilities, the MCCSS and MOH continue to pursue crisis-driven and reactive measures that do not address broader system needs or the growing demand for service.
142 The MCCSS primarily relies on the annual Multi-Year Supportive Living Planning (MYSLP) process to allocate new funding resources to build capacity and to transition priority individuals into funded services and supports. This process generally funds individuals on the community waitlist one at a time.
143 The groups prioritized for this funding include youth from the child welfare system (Crown wards) and children who were in receipt of complex special needs funding who are transitioning to and eligible for adult developmental services. All those identified each year in these two groups – who are considered to be at high risk of homelessness – must be supported to facilitate a seamless transition to adult services. Others who may be eligible for this funding fall within what is called the “community waitlist.” This group may include those who are inappropriately housed in hospital, transitional housing or shelters – or those who are homeless or at “critical risk” of homelessness. Funding allotment for prioritized people within the community waitlist depends on whatever is left over after the transition-aged youth receive funding.
144 As we saw in Luc’s and Kevin’s cases, Multi-Year Supportive Living Planning funding is often unavailable because allocations are delayed within the fiscal year, or the available money is insufficient to support individuals on the community waitlist, particularly if they have high needs. One official told us that the required housing and support costs for Luc alone would have “sucked up” all the funding for the entire region. In an internal MCCSS record prepared the day before Kevin was admitted to hospital, officials observed that given the number of adults with developmental disabilities in urgent need in the area, the Multi-year Supportive Living Planning funds would not cover the costs of those “who are inappropriately placed in hospital or in the community at the brink of relinquishment.”[47]
145 The unreliable schedule for allotting the funds each year also makes it difficult to plan. Ministry regional offices and planning tables might not be informed of the number of people that they can serve from community waitlists until months into the fiscal year. When funding is eventually announced, it is often insufficient for housing and support costs for identified individuals in urgent need. As a result, service providers and MCCSS regional staff are left scrambling to cobble together any resources for even temporary support.
146 Since 2020, the number of people that the annual planning process has supported from the community waitlist has been increasingly lower than the ministry-identified targets. MCCSS targets themselves also reflect only a small fraction of those in urgent situations who require funding for suitable housing and supports. For 2020-2021, the Ministry had initially identified that 250 inappropriately housed individuals would benefit from funding, but in-year targets for the entire community waitlist were set at 70, and ultimately 84 received funding. In 2021-2022, the Ministry increased its target from 120 to 150, based on urgent demand, and served 169 individuals. Unfortunately, this one-time increase did not come close to reversing the trend.
147 Over the next two years, funding for prioritized individuals on the community waitlist fell short of the targets. For 2022-2023, the target was 120, but only 20 people received funding. The next year, with the same target, only 60 received funding. The situation was even worse for 2024-2025. MCCSS had again targeted 120 new intakes from the community waitlist, but there was no funding for anyone on that list, and the Ministry was only able to fund prioritized transition-aged youth.
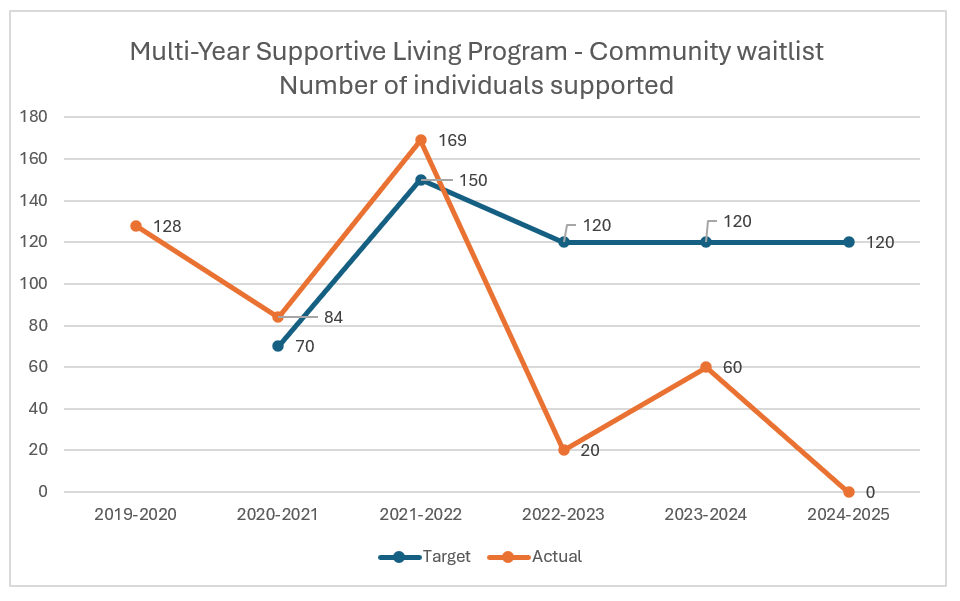
148 Ministry staff pointed to an increase in the number of prioritized youth transitioning to the adult system with increasingly complex needs as a reason for the decreasing funding available for adults prioritized on the community waitlist. Staff overseeing the Multi-Year Supportive Living program told us that higher inflation and more complex needs has resulted in the average supportive living cost increasing year after year.
149 The Ministry’s records reveal it is well aware that forecasted targets are insufficient and do not reflect the increasing pressures within the system, including the number of individuals inappropriately placed in hospitals, shelters, and jails.[48] They also cannot satisfy my recommendations from Nowhere to Turn to prioritize those living in unsuitable settings. One senior regional official described the multi-year planning process to us as “infinite need” with “finite resources.”
The more we work together: Dual Diagnosis Alternate Level of Care Project
150 The Dual Diagnosis Alternate Level of Care Project – jointly developed by the Ministry of Health and the Ministry of Children, Community and Social Services – is another example of a well-intentioned but reactive approach that resulted in a temporary Band-Aid rather than a long-term systemic solution. The project supported prioritized individuals with both a developmental disability and a mental health diagnosis in transitioning out of hospital. However, it primarily did so one at a time, without addressing broader system barriers.
151 The ministries told us the project was a reaction to two key developments. The first was a 2020 Ontario Court of Appeal decision that found that confining a man with significant physical, intellectual, and psychiatric disabilities to a forensic hospital for six years due to a lack of suitable housing in the community violated his right to liberty under the Canadian Charter of Rights and Freedoms.[49]
152 The other major factor was the COVID-19 pandemic, which amplified the need to free up hospital beds. Senior MOH staff said that they were also aware of two particularly “heart-wrenching” situations where people with developmental disabilities had spent several years in hospital. Despite collaboration with MCCSS, they were unable to find adequate funding or suitable community solutions for these individuals. They told us they knew they had to do something.
153 In 2021, each ministry was allotted $2 million from within existing budgets to help support individuals in transitioning out of hospital. In 2022-2023, the ministries each received $5 million for the year, and in 2023-2024, each was allotted $9 million for the project. The ministries created a “collaboration table” and working group composed of staff from both ministries and Ontario Health. Initially, the project aimed to reduce alternate level of care days in hospital, prevent avoidable emergency department visits, and remove systemic barriers where possible. The project goals evolved and narrowed to focus on transitioning prioritized individuals with a dual diagnosis out of hospital and ensuring they were able to stabilize in the community.
154 The Dual Diagnosis Alternate Level of Care Project was a positive step towards collaboration across the developmental services and health sectors. The stories of Noah, Jordan, Jack, and Kevin would likely have ended very differently if not for the funding and support available through this collaboration. Several officials we interviewed from the ministries and Ontario Health emphasized the project’s success in supporting selected patients in moving from hospital to the community. Since 2021, the project has been able to support at least 34 individuals in transitioning to a home and connecting to other needed health and behavioural services.
155 One Ontario Health official told us that moving just one person freed up hospital bed space for potentially hundreds of patients, because alternate level of care patients with developmental disabilities often occupy beds for years – beds that normally provide short-stay acute treatment in 3-5-day cycles.
156 The impact on individuals remaining in hospital cannot be overstated, given the negative effects of hospitalization on quality of life. One senior professional working in case management in the developmental services sector described the situation in bleak terms:
You’re dealing with a tragic story in our province of these people who are in hospital... There are some times when I deal with these cases I say to people only half-jokingly, that these people would be better off if we sent them to Guantanamo Bay than where they are right now….
[T]hey’re in the hospital room in restraints for… long, long periods of time with a security guard posted outside their door and nothing happening….
[T]hey’re living, breathing human beings, but their treatment is completely inhumane.
Not addressing the forest for the trees
157 Despite its individual successes, the Dual Diagnosis Alternate Level of Care Project had several limitations. It did little to address the underlying systemic causes that result in hospitals serving as default housing for individuals with developmental disabilities and complex needs.
158 The project’s Terms of Reference stated that alternate level of care patients with dual diagnosis remain in hospital because the right types of community-based services do not exist or are limited in terms of resources to support people with complex needs. From the outset, the project’s working group was aware of the systemic barriers to transitioning to the community. At an early stage, one working group member was recorded in meeting notes as saying, “a system approach to planning and facilitation is key to success. A large part of the issue is the system capacity, type of placement and limitations of resources.”
159 Despite this recognition, the project primarily focused on individual cases and did not address systemic barriers. These barriers delayed and prevented movement of eligible individuals out of hospital, and the project served far fewer individuals than originally contemplated. Initially, the ministries estimated that they could help about 50 people transition out of hospital by July 2022. In reality, 10 individuals were identified for the initial phases of the project and by April 2022, only two had transitioned out of hospital.
160 Transitions were stalled in 2022 because government funding was only approved on a fiscal, rather than annualized, basis and would not support individuals to move to permanent housing. It took more time to build and renovate supportive living spaces to meet individual needs than anticipated, and the budgets required to support individuals in the community were “significantly higher” than expected.
161 Several officials from both ministries told us they wished a more holistic or systemic approach had been applied from the outset, involving more planning and clearly articulated roles and responsibilities.
162 In February 2023, an internal MOH presentation set out the challenges the project faced, including the lack of affordable and accessible housing and community mental health supports.[50] It recommended shifting to a system approach. One MOH official involved in the project told us they believed that the project was doing “a lot of good” for individuals selected to transition from hospital, but feared that “we’re just gonna be in the same situation a few years from now if we don’t do something different in the system.” This official said their “biggest regret” was the reactive nature of the project and the lack of a “strategic piece.”
Limitations on eligibility
163 The narrow focus of the Dual Diagnosis Alternate Level of Care Project also limited who could be supported. Internal documents we reviewed show that MCCSS staff initially tried to broaden the scope to include those with complex needs generally but, from a MOH perspective, it was important to ensure health funds supported individuals with a mental health diagnosis. Professionals we interviewed in both the developmental services and health care sectors explained that the requirement that a person with a developmental disability in alternate level of care also have a formal mental health diagnosis excludes other long-stay patients with complex needs who face similar barriers to transitioning out of hospital.
164 One regional Ontario Health official told us more than half the long-term patients with developmental disabilities occupying a mental health bed in their area did not have a mental health or substance use disorder diagnosis.
165 We heard in interviews that there are various reasons for someone with a developmental disability not having a formal mental health diagnosis, even if they present with challenging behaviours, receive psychiatric treatment, and/or occupy a psychiatric hospital bed. Sean is an example of someone with very complex needs who does not have a mental health diagnosis, meaning he would not have been eligible for the project.
166 MOH staff we interviewed acknowledged that those without a mental health diagnosis likely face the same challenges in transitioning to the community as those who are formally diagnosed. Another senior Ministry official said there should be no barrier to collaborating to support individuals with developmental disabilities who do not have a mental health diagnosis, if they are in mental health beds and it affects access to care. As they put it: “We are one government and we’re collectively responsible for these individuals.”
Data limitations
167 Officials from both ministries acknowledged that the project had no access to reliable data on the number of people with a dual diagnosis in hospital. The numbers from Ontario Health and Developmental Services Ontario varied.
168 In early 2023, well over a year after the project began, the MOH began requesting and tracking Ontario Health data on alternate level of care hospitalizations for those with developmental disabilities. The aim was to assess monthly trends and inform project decision-making. However, MOH staff told us they did not know if the data reflected only those with a dual diagnosis, or those with developmental disabilities generally.
169 Based on the numbers they received from Ontario Health, the MOH found that the number of alternate level of care patients in hospitals was not decreasing. One official remarked to us: “Once someone goes out, boom, there’s someone else right in those beds.” Although the numbers are likely under-reported due to limitations in the system, the project initially estimated there were more than 70 individuals with developmental disabilities in hospital who were designated as alternate level of care. As of December 2024, the number had increased to 124.
170 The project’s success in meeting individual goals was not evaluated as required. It called for the ministries to prepare annual “activity reports,” but as of December 2023, these had not been produced. By January 2025, the ministries had developed a questionnaire to gather information from service agencies about their assessment of the transition process, including regarding communication, access to clinical services, and any learning opportunities. They anticipated sending it out sometime in 2025.
The end of the pilot project
171 Despite its limitations, the Dual Diagnosis Alternate Level of Care Project was a promising step towards a collaborative approach to this crisis. Unfortunately, the efforts seem to be over. MCCSS staff told us there was no commitment from the government to invest further in the project. They submitted a request for funding to expand the project in 2024-2025 to support transitioning up to 90 individuals out of hospital over three years. This funding was not approved.
172 MOH documents, along with some officials, have signaled a future intention to focus on systemic change and preventing alternate level of care hospitalizations. MOH and MCCSS staff said they are meeting regularly to discuss options to address and prevent long-stay hospitalizations from a system perspective, but no substantive plans have been developed at this point.
173 It is important that acute care beds within Ontario’s hospital system are available for those who need them. It is also imperative that individuals with developmental disabilities not suffer the indignity and hardship of prolonged and unnecessary hospitalization.
Planning for the future is long overdue
174 One MCCSS official observed to us that the current process of serving individuals one at a time does not develop needed system capacity. Another suggested that, ideally, supportive living planning would consider the needs of cohorts of individuals over “a multi-year horizon” and include earlier planning discussions with service agencies about creating options for individuals based on what the needs are.
175 The developmental services sector has been criticized for years for its reactive and crisis-driven planning approach. Successive recommendations for developing a supportive housing strategy targeted to those with developmental disabilities have gone unheeded. Without a comprehensive, needs-based, integrated supportive housing strategy and plan – and associated resources and cross-sector partnerships – the system will remain reactive. It will continue to leave people with disabilities institutionalized in hospitals or other inappropriate settings, waiting for suitable housing options to materialize. The multi-ministry initiative led by the Ministry of Municipal Affairs and Housing might help to address some of the supportive housing gaps in future, but this remains unclear.
176 The time for adopting a proactive approach to system planning in the developmental sector is long overdue.
177 In addition to working on solutions to the individual needs of those languishing in the hospital system, a systemic approach is necessary. I am recommending that the Ministry of Children, Community and Social Services and Ministry of Health establish a joint forum to engage in proactive system planning, including to address the lack of supportive housing for individuals with developmental disabilities and complex needs on a priority basis. There is already a wealth of research and recommendations relating to the challenges for long-stay patients to transition to suitable supportive housing in the community to guide the ministries in their planning.
178 This joint forum should be standing, rather than ad hoc. It should be formally recognized and supported within both ministries to ensure it is sustainable over the long term. The joint forum should be co-chaired by representatives from both ministries, have approved terms of reference, defined membership to include key developmental and health partners, and a regular meeting schedule. It should also have clear authority to develop a strategy to address the barriers that prevent people with developmental disabilities and complex needs from transitioning to suitable housing and support in the community. In the interest of accountability and transparency, and to support its long-term success, the joint forum should report to the Deputy Minister of Health and the Deputy Minister of Children, Community and Social Services, and provide a semi-annual progress update to the Ombudsman.
Recommendation 1
The Ministry of Children, Community and Social Services and the Ministry of Health should immediately establish a standing joint forum to engage in proactive system planning for individuals with developmental disabilities and complex needs. The forum should engage with any developmental services and health partners necessary for effective planning. The joint forum should commence its work no later than six months from the issuance of my report and should work collaboratively to address the barriers facing alternate level of care and long-stay patients with developmental disabilities and complex needs in transitioning to appropriate supportive housing in the community. The joint forum should report to the Deputy Ministers of each ministry and provide a semi-annual progress update to my Office.
Lack of capital funding
179 One barrier to finding supportive living resources in the community is the lack of capital funding to build housing capacity in the developmental services sector. Several people we interviewed told us that renting housing space for individuals with complex needs is often not possible because extensive renovations are required to incorporate safety and other specialized features. Without the necessary capital funding to create appropriate spaces, housing options remain limited.
180 Service agencies have sometimes been successful in obtaining minor capital funding through the MCCSS Partner Facility Renewal funding application process, for things like minor renovations and repairs, including for health and safety upgrades. However, one service agency told us obtaining this funding was “like winning the lottery.” Dedicated and adequate capital for home purchases or major renovations is even more difficult to access.
181 Service agencies expressed concern to us about what they perceive as government reluctance to fund physical spaces, leaving them to cobble together “piecemeal” funding to create needed and suitable housing for individuals with complex needs.
182 One service agency told us that they had land to build housing on, but there was no capital funding available. They criticized the government’s willingness to provide hundreds of thousands of dollars to renovate an apartment for one individual, but its reluctance to divert that same amount of funding toward purchasing or building new housing that could support more than one person. They commented: “[T]here has to be some type of visionary thinking as opposed to [a] one-off basis.”
183 As one Manager of Complex Case Coordination observed, the Community Network of Specialized Care does its work by advocating for clients and coordinating supports, but “the bottom line is…we don’t have the housing to transition the person into.” A November 2022 internal Ministry draft funding request for social services infrastructure and strategy described capital allocation as reactive and based on pressures that arise each year.[51] This document stated:
Without facilities such as … specialized clinical support for adults or group/supported independent living settings, more Ontarians are seeking treatment from hospitals or primary care physicians and will potentially stay longer as adequate supports cannot be secured post-treatment. The additional influx increases pressures on an already overburdened health services system.
184 One advocate we interviewed emphasized that, while there is a clear need to move away from large group settings that resemble the previous institutional model, the capacity issue needs to be addressed. They said, if the Journey to Belonging vision is not properly resourced, “the journey to belonging is actually [going to] be a journey to nowhere.”
185 To prevent this vision of the future, the MCCSS should proactively plan to develop and fund adequate and appropriate community infrastructure to support the needs of hard to serve individuals with developmental disabilities.
Recommendation 2
The Ministry of Children, Community and Social Services should include capital planning and funding as part of proactive developmental services system planning, in order to develop adequate and appropriate community infrastructure to accommodate the needs of individuals with developmental disabilities, including those with more complex needs.
Static funding in a world of increasing costs
186 The MCCSS typically does not account for inflation or an individual’s changing needs in its funding allocations in the developmental services sector. Over time, this practice has reduced the ability of service agencies to meet the increasing needs of those requiring supportive living in the community.
187 Typically, when a service agency has a vacancy, it is because a resident has died or moved to another home. The funding and staffing levels attached to the vacancy reflect the original arrangement established with the Ministry. Such funding arrangements can be decades old and insufficient to meet current staffing and living costs, let alone any additional needs of the new resident.
188 Many service agencies also expressed concern to us that they had not received an increase to their base funding for more than a decade. Said one Ministry official:
We’ve made our [developmental services] agencies operate on the same budget for 14 years, and you wonder why we can’t get people to develop and invest in resources for this type of scenario…. So now we react only to emergencies and crises. ... I’m... on the end of a fire hose every day in my region.
189 An MCCSS paper in 2019 confirmed that operating funding for developmental services transfer payment agencies had not increased significantly over the past 10 years. It observed that service agencies had also not received additional funding to address the increased support needs of their aging client base.[52]
190 In 2024, the MCCSS increased service agencies’ base budget by about 3% to help address some of the inflationary and wage pressures so they could maintain existing services. The increase was not intended to address increased needs or to build additional capacity in the system. As one service agency told us, the increased cost of living “gobbled all of that up.”
191 Service agencies can report financial pressures to the Ministry or submit a business case for one-time or ongoing additional funding. Obtaining such funding is dependent on available resources and is often a temporary fix rather than a permanent solution. Such funds are often scarce and inadequate to support increased needs of existing residents in supportive living, or a new resident coming into a home. If an agency is unable to access additional funding to meet a long-term resident’s increasing needs, that person might have to leave the only home and community they have known for much of their life.
192 Some Ministry and service agency officials told us a more transparent system is required to enable service agencies to request additional funding to address changing individual needs over time.
193 The MCCSS’ current practice relating to funding vacancies and base funding of service agencies in the developmental services sector disregard future cost increases, including through inflation. The sector is in a perpetual state of catch-up and crisis, scrambling for temporary fixes and temporary funds. As part of the proactive system planning I have recommended the Ministry engage in, it must develop a transparent process for negotiating increased funding when individual needs change. Such a process should include clearly defined eligibility and decision-making criteria that are clearly communicated across the sector. The MCCSS should also anticipate increases to service agency budgets and vacancy funding, and build planning for those increases into each funding decision. Planning should reflect realistic projections, rather than conditions that existed in the past.
Recommendation 3
The Ministry of Children, Community and Social Services should include financial forecasting of service agency costs and vacancy management as part of its proactive system planning.
Recommendation 4
The Ministry of Children, Community and Social Services should develop a transparent process for negotiating budgets to meet increased individual and service agency needs as part of its proactive system planning. This process should include clear eligibility and decision-making criteria that are provided to my Office and communicated across the sector.
It’s More than Housing: Cross-Sector Collaboration
194 Based on the cases we reviewed, several factors must come together for a successful transition from hospital to the community. Most of the people featured in this report required the collaboration of the MOH and MCCSS to fund housing, customized renovations to meet individual health and safety needs, and access to specialized clinical and/or behavioural services during and after transition. In some cases, collaboration and staffing support through private service agencies was also required.
195 Over the years, researchers and government officials have recognized the need for integrated, collaborative approaches to support people with developmental disabilities, including to prevent inappropriate hospitalizations and to facilitate transition from hospital to the community.
196 For example, in 2017, an independent consultant funded by the MCCSS and a Local Health Integration Network reviewed a pilot project involving a “cross-sector complex care model” and explored how to support people with developmental disabilities and medical complexities. The consultant found that individuals with developmental disabilities may find themselves stuck in hospital or long-term care when there is nowhere for them in the community and that a siloed approach will not address the problem:
Neither the developmental services sector nor the health sector is equipped, on its own, to support these individuals. Instead, there is a need for a proactive integration of resources and services to support these individuals and their families through the lifespan, and to avoid health crises along the way.[53]
197 The Centre for Addiction and Mental Health published several reports from 2009 to 2023 that underscored the importance of co-operation and collaboration between the health and developmental service sectors to help people with dual diagnosis transition from hospital to the community. The Centre’s 2019 report, Addressing Gaps in the Health Care Services Used by Adults with Developmental Disabilities in Ontario[54] describes poor health outcomes for individuals with developmental disabilities and their increased risk of repeat hospitalizations. It emphasizes that successful discharges for such individuals require coordination, not only between hospitals and the community, but also across different funders and sectors: “[B]ecause adults with [developmental disabilities] need and receive services and supports from both the health and social services sectors, intersectoral co-operation is essential...”.
198 More recently, the Centre’s 2023 practice guidance on Supporting Alternate Level of Care patients with Dual Diagnosis to Transition from Hospital to Home[55] explains the importance of coordinated access to any required developmental, medical and clinical care – including primary care, psychologists, behavioural therapists, social workers, nurses, and speech and language pathologists. The Centre recommends the same approach for other populations, such as people with developmental disabilities who have complex medical needs or those with “distressed behaviours” unrelated to psychiatric issues.
The struggle to access developmental supports in hospital
199 In many cases, cross-sector collaboration and care is important to successful discharge even while individuals with developmental disabilities remain in hospital. Some of the stories featured in this report illustrate how in-hospital developmental and behavioural services can help mitigate the loss of skills and the effects of institutionalization. They can improve quality of life and facilitate communication between patients and hospital staff, all of which improves the likelihood of an eventual successful transition to the community.
200 For instance, the service agency that was eventually engaged to provide in-hospital developmental supports to Noah observed that he was not aggressive when he was admitted to the hospital, but because he was not understood and he did not understand what was happening, his behaviours “snowballed” and use of restraints increased over time.
201 Lack of consistency in developmental support in hospital can also disrupt patient progress and wellbeing. In Luc’s case, when the hospital did not renew its contract with a developmental service agency that was supporting him, his eating decreased significantly and there were 24-hour periods when he ate nothing.
202 Developmental service agencies we spoke with emphasized the importance of getting direct-support professionals in hospitals as soon as possible. They noted it takes time to build trust and relationships to understand what a person is experiencing and what their needs are – and then to help them become “community-ready.”
203 Unfortunately, there is no mechanism within either the MOH or the MCCSS to fund consistent, timely, and equitable access to these services. MCCSS officials told us that typically a hospitalized person needs a transition plan and an agency actively planning for them to get funding and access to developmental supports in hospital. As the cases in this report demonstrate, it can take months to find a service agency willing and able to support transition to supportive living. Even when an agency is involved, it might not have enough staff to provide in-hospital care.
204 People who have Passport funding can use it to hire direct-support professionals. However, as happened in Jordan’s case, even the maximum funding amount is often insufficient to cover the support needed over an extended hospital stay. To complicate matters, some hospitals do not permit developmental support staff or outside agencies to assist patients.
205 As a result of this patchwork approach, access to developmental support can be markedly different from case to case. For example, Luc and Noah lived on the same hospital ward at the same time, and although both went through periods without developmental assistance, there were times when Luc received full-time behavioural support as well as 24-hour assistance from two developmental support staff. Noah had only one developmental support worker for six hours a day, despite having higher-rated support intensity needs. A service agency familiar with the situation told us they believe this reflected an inequitable allocation of resources.
Ongoing clinical and behavioural supports
206 The availability of appropriate clinical supports during transition and post-discharge is often important to the successful, sustainable transition of patients with developmental disabilities and complex needs to the community. One developmental service agency told us clinical expertise, such as behavioural consultation and service in the community, can help ensure the individual, support staff and any others in the home are safe during crisis periods, potentially preventing reliance on police and hospital re-admission. They also said that, without access to a physician, agencies may have to return to emergency departments just to get a prescription refilled.
207 Coordination between the MOH and MCCSS can help to ensure that individuals have access to funded transitional clinical supports. For instance, in Sean’s case, his condition is simply not manageable in the community without ongoing medical and nursing support. Noah, Luc and Kevin required psychiatric and behavioural supports to facilitate transition out of hospital. Unfortunately, the level of involvement by the MOH and the specialized clinical and behavioural supports that they received throughout the transition process were unusual or unheard of, according to several witnesses we interviewed.
208 Apart from the Dual Diagnosis Alternate Level of Care Project and the Dual Diagnosis Transitional Rehabilitation Housing Program[56] for forensic clients, collaboration to support people whose needs traverse the two systems is limited. The two ministries have a joint Exceptional Care Memorandum of Understanding that can be used to support people with developmental disabilities who have high and complex needs. The memorandum states that the need for greater collaboration and service integration is particularly important for individuals with developmental disabilities, to ensure services will be “available and accessible at the right time and in the right place.”
209 Despite this agreement, collaboration between the ministries to support and provide funding for these individuals tends to be limited and ad-hoc.
210 Since 2015, the ministries have only collaborated to fund five individuals under the Memorandum. One of those lived with a developmental disability, was deafblind, and lost the ability to walk after remaining in a hospital bed for a year, due to lack of sufficient support and medical care in the community. He finally received funding for the support he needed to return to the community through an Exceptional Care agreement, but this was only made possible after a senior executive with a developmental service agency pleaded with the MCCSS for weeks for a funding solution to help this man leave hospital.
211 The particular agency was also able to support this man’s complex medical and developmental needs because they are one of a limited number of developmental service agencies in Ontario that directly hire and have medical and behavioural specialists embedded in their supportive living service. Sixteen such developmental service agencies are part of the Specialized Clinical Developmental Services Network – they typically do not receive Ministry of Health funding but often support those who are medically fragile or require intensive behavioural supports.
212 Other service agencies we spoke with described challenges in accessing transitional or post-discharge clinical supports from hospital, and an overall lack of integrated person-centred care. One developmental service agency executive remarked that although some hospitals have accommodated requests for clinical supports to continue once the person is discharged, others have been unwilling or unable to do so. Some described a “dividing line at the hospital doors.” Once the patient is discharged, clinical support ends. This can result in repeat unnecessary hospitalizations or contribute to the collapse of a supportive living arrangement.
Failing to coordinate is planning to fail
213 Internal guidance documents for administering MCCSS’s Multi-Year Supportive Living Planning process emphasize the need for developmental service agencies to build on or establish linkages with sector partners such as local health partners, Ontario Health Teams, and community mental health agencies.[57] However, we heard from multiple officials from MCCSS and the health and developmental service sectors that this generally does not happen in practice, either to prevent hospital admission, during hospital stays, throughout the transition process, or post-discharge.
214 In 2020, a KPMG report[58] to the MCCSS on improving effectiveness of developmental services found there was no formal network for integrating services within the developmental services sector or between developmental services and adjacent services, such as health.
215 In 2021, internal MCCSS documents stated they still did not have a viable cost-sharing agreement with the Ministry of Health that would enable collaborative funding arrangements.[59] The same year, MCCSS policy staff prepared a presentation on “health access barriers” and observed that the COVID-19 pandemic further exacerbated pre-existing health and mental health challenges.[60] The presentation notes that the pandemic highlighted system issues such as poor connections between sectors and lack of prevention and proactive supports. While acknowledging that the MCCSS had been working with the MOH to move alternate level of care patients with developmental disabilities out of hospital, policy staff flagged that more preventative solutions might be required.
216 Health and developmental services professionals we spoke with recognized the need for more integrated solutions to support the successful transition of individuals with complex needs out of hospital. Some MCCSS officials suggested that the MOH could have a greater role in ensuring access to clinical supports, such as mental health services. One MOH official agreed that without community-based services, including mental health supports, those who leave hospital will likely end up back there. Others recognized that the MOH could have a role in funding transitional supports, but cautioned that further research is necessary. They observed a better understanding of the profile and requirements of people in extended hospitalizations and better data on the numbers affected were needed.
217 Although having accurate data on the demand for these services is important, the need for integrated supports across the developmental services and health sectors is not a novel idea. A 2008 Joint Dual Diagnosis Policy Guideline[61] set out a vision for providing integrated, coordinated, and proactive mental health and developmental services to people with dual diagnosis and their families. Integrated care is required beyond mental health care. In a 2012 Provincial Review of Dual Diagnosis Programs[62], KPMG proposed more integrated care, including development of a community model. It envisioned hospitals supporting community services, shared resources and information, virtual beds, mobile/outreach teams, joint services, and a Dual Diagnosis Tertiary Care Committee to oversee and facilitate a “strategic integrated approach.”
218 In a 2018 presentation[63], the MCCSS identified several short and long-term strategies to better integrate services. The options included expanding the role of health professionals to better serve people with developmental disabilities in such areas as primary care, nursing and home care, promoting community capacity through health investment in professional development programs for health professionals, and establishing a formalized commitment between MCCSS regional offices and Local Health Integration Networks (now part of Ontario Health).
219 In 2021, one Local Health Integration Network developed a draft Dual Diagnosis Clinical Model and Template Framework in response to two troubling cases of patients with developmental disabilities who had been hospitalized for extended periods. The goal of the framework was to create an ideal model of care and pathways for alternate level of care patients or those with intellectual and developmental disabilities who are at risk of hospitalization. It envisioned a multi-organizational model of care in the community with a core team of professionals to help prevent hospitalization and overcome “siloed” care. Additional reports and submissions to the MCCSS have recommended a similar “multi-disciplinary” approach.
220 Despite the documented universal recognition of the importance of integration and collaboration across the developmental services and health sectors, the systems still largely operate in isolation. Throughout this investigation, we heard from professionals and officials from both sectors that services and supports remain fragmented and “siloed,” and that this is a significant barrier faced by individuals with developmental disabilities and complex needs in transitioning to the community.
221 Witnesses from the respective sectors talked to us about the friction that exists when there is no shared sense of purpose in addressing the needs of patients with developmental disabilities. Developmental services sector professionals told us that “there’s a lot of blame” when both ministries are involved. They said the sense is that “it’s someone else’s problem,” there is a “silo mindset”, and there is “no standard understanding that we’re working in this together....”
222 I have already recommended that the Ministry of Children, Community and Social Services and Ministry of Health establish a standing joint forum to collaborate on planning for this sector. This forum should also work towards identifying and implementing integrated services and supports across the developmental services and health sectors to prevent unnecessary hospitalizations and support patients with developmental disabilities in hospital, as well as through and after their transition to the community.
Recommendation 5
The Ministry of Children, Community and Social Services and the Ministry of Health should work together, through the joint forum referred to in Recommendation 1, to identify and implement an integrated approach and appropriate care framework for delivering services and supports across the developmental services and health sectors to prevent unnecessary hospitalizations and support patients with developmental disabilities with complex needs in hospital, during transition, and post-discharge in the community.
223 The two ministries should also provide further guidance to hospitals and developmental service agencies about the importance of developmental services and supports for patients in hospital and the provision of clinical supports, including any needed clinical training for developmental service agencies, during transition and post-discharge. The joint forum I have recommended that the ministries develop should address elimination of the current barriers that prevent patients from receiving necessary direct support services while in hospital, and work to support the provision of clinical supports necessary for a smooth transition of patients into the community.
Recommendation 6
The Ministry of Children, Community and Social Services and the Ministry of Health’s joint forum, referred to in Recommendation 1, should work towards ensuring patients have access to necessary developmental supports while in hospital and clinical supports during and after transition to the community.
Reframing the Joint Dual Diagnosis Policy Guideline
224 The idea of a joint ministry effort to address services for people with developmental disabilities is not new. For years, there has been a guideline for the ministries to work together to develop and facilitate access to integrated supports for those with a dual diagnosis. The MOH and MCCSS initially drafted the Joint Policy Guideline for the Provision of Community Mental Health and Developmental Services for Adults with a Dual Diagnosis in the late 1990s. The ministries last officially updated the guideline in December 2008.
225 The guideline was intended to strengthen community capacity to support the needs of those with both a developmental disability and mental health diagnosis. One of the guideline’s “key assumptions” is that cross-sector collaboration is essential at all levels to provide appropriate services. However, when we asked MOH and MCCSS officials about actions taken to advance the 2008 guideline’s goals, the majority we spoke with were unable to point to any tangible steps, or were unfamiliar with the document.
226 While well-intentioned, the guideline did not achieve its intended purpose. Ministry documents[64] state that a 2012 evaluation of the guideline found a lack of shared ministerial commitment and unclear roles and direction, along with a lack of accountability or structures to support implementation. The evaluation recommended developing an inter-ministerial framework to focus on better coordination of supports for people with dual diagnosis and greater accountability.
227 Between 2013 and 2015, staff from both ministries, along with various health, dual diagnosis, and developmental disability experts, worked together as part of a Dual Diagnosis Framework Working Group to revise the guideline and create a new framework. The group completed a draft in 2015. However, the Working Group never published the framework and revisions continued, resulting in a second draft in 2017. It included the statement: “Current resources need to be re-evaluated and transformed to seamlessly deliver evidence-based, proactive services, as appropriate.” It again emphasized the need for transitional support for those transitioning from hospitals or other institutions and protocols for service agencies to work together to provide such services.
228 MCCSS records show both ministries approved the 2017 framework for “engagement purposes.” However, the ministries essentially shelved the document. An internal MCCSS record from 2018[65] suggests the ministries did not release the proposed framework because they believed there would be opportunities to address system access and integration through the government’s commitment to invest $3.8 billion over 10 years in the sector and create a “comprehensive and connected service system.” MCCSS anticipated there would be “some version of a Dual Diagnosis Framework” in future, but there were questions as to how it would be “recalibrated.”
229 Ministry emails show that in January 2022, a senior MOH official contacted their counterpart in the MCCSS to discuss revisiting the framework. The ministries eventually assigned the task of updating the document to the Dual Diagnosis Alternate Level of Care Project working group. However, as of early 2025, this work had yet to be completed.
230 The absence of clear roles and responsibilities across the two ministries continues to present challenges. MOH officials in particular have emphasized to us the importance of clarifying the respective roles of developmental services and the health sector before attempting to address system gaps. We reviewed an email exchange between the ministries about the unavailability of psychiatric support needed to facilitate transitions for individuals leaving hospital. MOH staff replied that there was no commitment from their Ministry that psychiatrists would follow individuals into the community and suggested that if a hospital agreed to do so, it was a “local negotiation.” MCCSS staff replied: “I guess this is where a [Dual Diagnosis] Framework would come in handy...?”
231 To facilitate collaboration and planning at the individual and system level, I am recommending that the Ministry of Children, Community and Social Services and the Ministry of Health work together as a priority to update, publish, and implement the Dual Diagnosis Framework.
Recommendation 7
The Ministry of Children, Community and Social Services and the Ministry of Health should, as a priority, work together to update, publish, and implement the Joint Policy Guideline for the Provision of Community Mental Health and Developmental Services for Adults with a Dual Diagnosis.
232 As demonstrated by the limitations of the Dual Diagnosis Alternate Level of Care Project, there are many reasons why an individual with a developmental disability in alternate level of care may not have a formal mental health diagnosis, despite having similarly complex needs. The ministries should expand the scope of the framework to include individuals with developmental disabilities and complex needs who do not have a formal mental health diagnosis.
Recommendation 8
The Ministry of Children, Community and Social Services and the Ministry of Health should extend the application of the Joint Policy Guideline for the Provision of Community Mental Health and Developmental Services for Adults with a Dual Diagnosis to individuals with developmental disabilities and complex needs who do not have a mental health diagnosis.
Behind the Curtain: The Mystery of Developmental Services
233 It is difficult to provide a person-centred integrated transition plan for individuals to successfully transition out of hospital when there is limited understanding within the health sector about the developmental services system.
234 Professionals in both the developmental services and health sectors suggested to us that the mystery surrounding the developmental services sector contributes to prolonged inappropriate hospitalization of adults with developmental disabilities. They described the developmental services system as overly complex, opaque, and difficult to navigate. One experienced hospital staff member said they have had to accumulate knowledge case-by-case, without any guidance. In fact, some hospital staff we interviewed had no familiarity with the developmental services system or DSO.
235 One hospital professional who worked with Jordan said he was the first alternate level of care patient she had ever encountered and she had no idea what DSO was or why it was important to notify them about Jordan’s case. Those working to get Jack back to the community told us they thought they had done well when, after several years in hospital, they had managed to add his name to the DSO registry for supportive living. It was years later when they discovered that getting on the list was only the first step, and accessing supportive living would be a multi-year process.
236 A health researcher with experience in both the developmental services and health care systems commented that results largely depend on whether there is someone with knowledge of the system available to advocate on behalf of an individual patient:
[T]he pathways and how to get resources... are often very unclear or nonexistent or just very variable. And the result is that people who have strong advocates – whether that's a family member or whether that's a staff member in the hospital or in the community sector… who happen to be strong advocates, who happen to know something about the system, or happen to have good relationships with people in the system – are the ones who often end up having better outcomes.... And I think that's … just very upsetting.
237 Many medical professionals and hospital social workers we spoke with said they would welcome having more information and training about developmental services planning and funding processes. However, some MOH officials said such training might be unrealistic for emergency department personnel, given the urgent and sometimes overwhelming nature of their work.
238 Ontario Health staff told us that during the pandemic, many hospitals lost experienced staff who were familiar with the developmental services sector, such as discharge planners and care coordinators. One Ontario Health regional staff member said they were currently seeing a “real breakdown” in communication between hospitals and DSO.
239 DSO has periodically sent information and posters to hospitals. In 2023, it began developing a communication strategy for hospitals. In March 2024, DSO mailed information to 239 hospitals about its role and developmental services, targeting the materials to social workers and other hospital staff who are well-positioned to disseminate the information. DSO also provided information to other health care teams and professionals, including the Ontario Hospital Association, which shared information with its 3,875 members. Local DSO offices also do their own outreach and provide presentations to health care staff.
240 In response to my Nowhere to Turn report, the MCCSS also distributed information to hospitals about the developmental services sector, including contact information for DSO. However, significant knowledge gaps between the developmental services and health care sectors persisted.
241 DSO staff involved in communications told us they have provided outreach, education, and support to the health sector, but collaboration usually happens when there is a champion within a hospital. They noted that such contacts are valuable when discussing scenarios for alternate level of care patients with developmental disabilities. They said personal outreach and relationship-building between developmental services and health care remains an important component.
Lack of transparency
242 The lack of specific details about available supports and services also frustrates efforts to transition patients into appropriate community settings.
243 A senior hospital official working in a mental health unit in a large hospital told us the lack of transparency about wait times for supportive living hinders the hospital’s ability to plan for care or appropriate discharge. The official observed that “no one should have to live in a hospital.” And, given the limited resources and information about wait times and vacancies for supportive community living, they said hospitals are forced to consider “horrible” solutions.
244 The official gave the example of two men in their 20s who live with autism spectrum disorder. One had been in hospital for over a year; the other for several months. In one case, the hospital was pushing to transition the young man to a long-term care home for seniors – a terrible fit, but “better than the alternative of remaining in hospital indefinitely.” The hospital was considering discharging the other man to a shelter, despite the “moral distress” this option caused hospital staff, given that he could not care for himself without substantial support.
245 The hospital official suggested that the MCCSS share information on its website about the number of people waiting for supportive living spaces in the community and the number of spots that become available every month, so hospitals can better plan and manage family expectations.
246 Other hospital administrators told us that, given the limited information available about developmental services and supports, they often turn to private agencies or shelters because these resources are the only ones they can locate. One health sector official described the options available through the developmental services sector as “a black box.” Others, including experienced developmental service agency staff, used similar phrases, referring to the system as a “black hole” and “hidden system.” One professional used an analogy inspired by the Wizard of Oz, saying that the developmental services system exists “behind the curtain.”
247 When we asked MCCSS officials about the lack of transparency regarding the availability of supportive living and other developmental services in the community, they said it is challenging to share accurate information because the DSO database is limited, priorities constantly change in response to crises, and the registries continue to grow as new names are added.
248 There is a similar lack of easily accessible information about MOH-funded supportive living. As noted by Ontario’s Auditor General, the MOH does not collect waitlist and wait time information for supportive housing that it funds. The MOH has said that some of this housing can serve people with a dual diagnosis. More information about which homes provide support to individuals with dual diagnosis and their wait times would assist those involved in transition planning.
249 While there may be challenges in identifying the available supportive living accommodations at any given point in time, the MCCSS and MOH should publish meaningful information about waitlist numbers for supportive living options that can serve those with developmental disabilities/dual diagnosis, potential wait times, the number of annual vacancies that arise, and the number of people served by each supportive living type. Transparency is crucial to enabling system partners to work together to plan for transitioning people who are trapped in hospital to appropriate housing and supports as quickly as possible.
Recommendation 9
The Ministry of Children, Community and Social Services and the Ministry of Health should publish and annually update meaningful information on their websites about waitlist numbers for Ministry-funded supportive living, potential wait times, the number of annual vacancies that arise, and the number of people served by each funded supportive living type.
250 The limited availability of suitable supportive housing and other necessary services is a significant barrier to alternate level of care and long-stay patients with developmental disabilities in transitioning to the community. However, more education and training of hospital sector partners on the developmental services system, including relating to supportive living options and other services, would better prepare hospital administrators and other health professionals for discharge planning. I understand that DSO has made efforts in this area. However, to complement and build on this initiative, the joint ministry forum I have recommended should oversee the development and implementation of an ongoing education and training program. The program should be focused on providing information about developmental services system resources, programs, and processes to help hospital administrators and other partners plan for patients with developmental disabilities to transition to the community.
Recommendation 10
The Ministry of Children, Community and Social Services and the Ministry of Health, through the joint forum referred to in Recommendation 1, should work together to develop and implement an ongoing education and training program for the health sector, focused on providing information about developmental services and dual diagnosis resources, programs and processes, to assist with discharge planning for patients with developmental disabilities.
Communication and collaboration
251 Several witnesses stressed to us that the lack of formal protocols governing communication between developmental services and health partners often leads to inconsistent communication and undermines collaborative efforts.
252 A senior MOH official explained that, without a formalized communication process, successful collaboration between health and developmental services generally relies on the “personalities and people who’ve developed relationships” – and is lost when staff move on. The health official noted that although the MOH and the MCCSS have made efforts to collaborate, including through the Dual Diagnosis Alternate Level of Care Project, there is still a need for formal structures, policy directives and guidelines.
A seat at the planning table
253 The communication mechanisms that do exist and could facilitate cross-sector communication and collaboration do not operate uniformly and often exclude key partners. For example, participation by health partners at community planning tables is inconsistent across the province. MCCSS officials told us some planning tables have found a way to engage health partners in the planning process, while others have not.
254 Some hospital staff involved in care and discharge planning for patients with developmental disabilities told us they did not receive invitations to attend planning tables, while we heard from developmental services agencies and Ministry staff that some health care partners did not attend the tables when they were invited.
255 In Jack’s case, because hospital staff who worked with him and were planning his discharge were not included at the planning table, they were not aware that service agencies had been bypassing Jack for years, believing they could not manage his compulsion to consume water. Had they had a place at the table, they could have explained his positive attributes and how the hospital had successfully managed this behaviour. In their view, the agencies at the table need to see that the individuals being discussed are not just names. A developmental services agency official we spoke to confirmed it is important for people who know the individual to be at the planning table. Otherwise, they noted, service agencies make decisions based on “what’s on paper,” and some individuals come across as very challenging in writing.
256 The more high-needs an individual appears, the more reluctant service agencies generally are to offer support. For instance, in Noah’s case, DSO reassessed his support needs based on his behaviours and medical needs after he had been in hospital for almost a year, and in restraints for a significant portion of that time. The resulting rating was at the maximum level for support – something DSO and case management staff said they had never seen before. A developmental service agency familiar with Noah said that this would be very daunting for service agencies. It was important for someone who knew Noah to be at the table to explain that the assessment did not reflect his behaviours when he lived in the community, where he had been more independent.
257 Some MCCSS officials and developmental services staff agreed that it would be beneficial if hospital staff familiar with patients with developmental disabilities attended developmental services planning tables.
258 In addition, some developmental services officials we spoke with stressed the importance of sector representation and active participation at Ontario Health Team discussions to ensure that issues affecting individuals with developmental disabilities are highlighted and considered. One developmental services official we spoke with explained the importance of these collaborations:
If we're not at Ontario Health planning tables, and if they're not at developmental services priority and planning tables, then being able to develop systemic pathways and processes in a consistent way across the province is going to be really challenging.
259 On the other hand, MOH officials we spoke with questioned how helpful developmental services involvement in Ontario Health Teams would be in practice, given competing priorities and the breadth of medical issues addressed by the teams.
260 The need for greater cross-sector participation in planning tables has been recommended before. In 2023, the Centre for Addiction and Mental Health recommended that a consistent protocol be established across all developmental service regions to ensure hospital staff can attend developmental service sector committees, especially priority-setting meetings where current and future alternate level of care clients can be discussed proactively.[66] The same year, the Provincial Network on Developmental Services‘ Health Strategy and Engagement Working Group made similar recommendations.[67] The Network found that the lack of a formal or consistent framework for regular engagement between health service providers, planning entities, and developmental services limited effective collaboration that would support solutions for alternate level of care patients with developmental disabilities.
261 A failure to consistently include all interested parties in existing forums for cross-sector discussions has led to lost opportunities to share important information, and in some cases, left people in hospital for longer than was necessary. Additional ministerial guidance is required to ensure more consistent cross-sector collaboration.
Developing a joint protocol
262 Developmental services and health sector partners might disagree on the specifics of how structured collaboration should take place. However, those we interviewed generally agreed that effective planning for alternate level of care and long-stay patients with developmental disabilities requires a formal standardized process for communication and collaboration.
263 Some hospital staff we spoke with also contrasted the vague process of transitional planning for patients with developmental disabilities with the systems that currently exist for discharging patients to long-term care or addiction services. A few said standardized agreements or a memorandum of understanding between hospitals and developmental service agencies would be useful in governing the transition process, including a commitment to collaboration, transition preparation steps, a crisis plan in worst-case scenarios, and identification of transition team members.
264 I am therefore recommending that the joint forum I have recommended the two ministries create develop a formal protocol to govern communication and participation in discussions concerning patients with developmental disabilities. The protocol should include provisions for notifying DSO when such patients are admitted and when they become long-stay or alternate level of care patients. It should also set out a communication framework for transition and discharge planning discussions. It should clearly set out the respective roles, responsibilities, and expectations for developmental services and health partners and provide for participation of relevant hospital staff at planning table discussions.
Recommendation 11
The Ministry of Children, Community and Social Services and the Ministry of Health, through the joint forum referred to in Recommendation 1, should work together to develop and implement a joint protocol governing communication concerning patients with developmental disabilities, including around notification of Developmental Services Ontario when such patients are admitted and become long-stay or alternate level of care, and to support transition/discharge planning.
Recommendation 12
The Ministry of Children, Community and Social Services and the Ministry of Health’s joint protocol, referred to in Recommendation 11, should clearly set out the respective roles, responsibilities, and expectations for developmental services and health partners, and provide for participation of relevant hospital staff at planning table discussions.
265 The Ministries should encourage greater communication between health and developmental services sector professionals on issues of mutual interest through an appropriate, structured mechanism.
Recommendation 13
The Ministry of Health and the Ministry of Children, Community and Social Services should encourage increased communication between health and developmental services sector professionals concerning issues of mutual interest through an appropriate, structured mechanism.
Effective information sharing
266 Concerns about patient confidentiality can prevent important information sharing between the developmental services and health sectors. MCCSS and MOH must work together to develop an effective method of collecting and sharing necessary planning information about alternate level of care and long-stay patients with developmental disabilities.
267 In the case of planning tables, an MCCSS official told us that even if health partners do attend the tables, they are sometimes reluctant to share a patient’s personal medical information because of privacy considerations. They explained that DSO is not under the MOH’s “circle of care,” which allows free exchange of information, and if key health information is not disclosed at the planning tables, it can detrimentally impact efforts to transition individuals out of hospital.
268 One senior hospital official suggested that a possible solution to foster communication among hospital psychiatrists and community care providers, case managers, and behavioural therapists would be to turn developmental services organizations into health information custodians and allow them to share clinical information through Connecting Ontario, the provincial health records system. Others we spoke with suggested that an information-sharing portal specific to the health and developmental services sectors would be ideal.
269 As part of the work on the joint protocol I have recommended that they develop, the ministries should incorporate a method for relevant information sharing to facilitate discharge planning for individual patients. When developmental services and health partners do not share information critical to transitioning patients from hospital because of confidentiality concerns, individual patients suffer. I recognize that this might require a legislative solution.
Recommendation 14
The Ministry of Children, Community and Social Services and the Ministry of Health’s joint protocol, referred to in Recommendation 11, should include specific provisions relating to the sharing of patient information to facilitate transition planning for individuals with developmental disabilities.
Measuring the problem when the numbers don’t add up
270 It is difficult to know how many individuals with developmental disabilities in Ontario are experiencing similar conditions to those endured in hospital by Jordan, Noah, Luc, Sean, Kevin, Jack, and Anne.
271 The developmental services and hospital sectors both collect data about patients with developmental disabilities in hospital. However, they do so through two different information systems: Ontario Health’s Wait Time Information System and DSO’s Developmental Services Consolidated Information System. Neither fully captures reliable data about this population.
272 Without accurate, reliable data, it is difficult for ministries to move toward a data-driven approach to addressing the factors that contribute to inappropriate hospitalizations of individuals with developmental disabilities. When DSO does not have accurate and current data about them, they could miss out on needed services and remain in hospital even longer.
Wait Time Information System
273 Ontario Health’s Wait Time Information System is a web-based database that captures information and statistics on alternate level of care patients.
274 The system has several limitations when it comes to reporting on individuals with developmental disabilities. Its data field for when someone has “developmental requirements” that are a barrier to discharge – called the “Specialized Needs and Supports” field” – is underutilized by staff entering the data. Hospital staff we spoke with said there is a “high likelihood” that the number of alternate level of care patients with developmental disabilities is under-reported.
275 This may happen because physicians who are responsible for designating someone as alternate level of care may not be aware that the patient has a developmental disability. For instance, hospital staff did not recognize that Jack had a developmental disability for close to five years.
276 Hospital staff also might not view a developmental disability as a barrier to discharge but as a community resources issue. Hospital staff and clinicians may not understand the importance of reporting such information if it doesn’t relate directly to patient care. In addition, the Specialized Needs and Supports section is not a mandatory field.
277 Another major factor affecting the reliability of alternate level of care data on individuals with developmental disabilities is that there is considerable variation in practices among physicians and hospitals in designating patients as alternate level of care. For example, neither Noah nor Luc was formally designated as alternate level of care, even though clinicians recognized that the hospital was not a suitable environment for them.
278 In Jordan’s case, it took more than seven months for the hospital to designate him as alternate level of care. Hospital staff agreed that he did not require hospital level care shortly after his admission, but they believed there could be negative consequences of deeming him alternate level of care. For instance, Jordan may not have been considered for private behavioural treatment to help address challenging behaviours if he was considered “stable.” The delay in being designated alternate level of care affected the urgency with which the developmental sector addressed his circumstances. Service agency staff who worked with Jordan said it was only when he was officially designated alternate level of care that DSO increased his prioritization score and more detailed planning to provide him with services and supports began.
279 Ontario Health staff are aware that the Specialized Needs and Supports data field is underutilized and that alternate level of care designation practices vary. Ontario Health publishes an Alternate Level of Care Reference Manual that explains the data fields, and staff told us they have regular conversations with hospitals to encourage them to report on individuals with developmental disabilities. However, as MOH staff explained, hospital staff have many competing priorities that affect reporting and there is no formal guidance on the importance of reporting when someone with a developmental disability is in hospital. Officials suggested that the accuracy of the data might increase through greater education, training, and making the Specialized Needs and Supports section of the Wait Time Information System mandatory.
280 Currently, the MCCSS does not appear to use the data reflected in the Ontario Health reports in any system planning. One regional Ontario Health official commented to us that the data around alternate level of care patients with developmental disabilities was “really kind of meaningless” and raised more questions than answers, as it does not clearly identify individuals with developmental disabilities, or their associated health conditions and needs.
Developmental Services Consolidated Information System
281 DSO tracks information about individuals registered for services through the Developmental Services Consolidated Information System. DSO relies on service agencies, individuals, family members, caregivers, or hospitals to notify them when someone with a developmental disability is hospitalized. Timely notification is important because circumstances affect an individual’s prioritization, which can determine if and when they can access particular services.
282 There are various factors that affect the accuracy of DSO’s information. Some MCCSS officials we spoke with said the lack of a formal requirement or procedure for hospitals to contact DSO was problematic, and that written policies or practices for hospitals to follow would be helpful to improve communication and capture alternate level of care numbers. Some MOH and Ontario Health staff said there is reluctance to add to the “reporting burden” of hospital staff, particularly in smaller hospitals. However, smaller hospitals are more likely to lack the resources necessary to assist patients with developmental disabilities and would benefit from early notification to DSO to connect to support services.
283 When DSO is notified that someone with a developmental disability is in hospital because there are insufficient community services to meet their needs, the DSO system has no specific setting or field to enter that the person is alternate level of care or inappropriately housed. There is also no clear definition of when someone is considered “inappropriately housed.”
284 In 2017, the MCCSS worked on a draft definition of “inappropriately housed,” which was refined in 2019. However, the Ministry never adopted the definition. Three years later, senior DSO staff again flagged to the Ministry that the lack of a definition for “inappropriately housed” was contributing to inconsistency in reporting on individuals with developmental disabilities in hospital.
285 Given the limitations of the Developmental Services Consolidated Information System, some DSO offices keep a manual list of individuals they know are alternate level of care. However, even then, office staff we spoke with acknowledged that such lists are not necessarily current.
286 When it was developing the Dual Diagnosis Alternate Level of Care Project, documents we reviewed show that the MCCSS considered undertaking an alternate level of care “data quality improvement plan” and again considered incorporating a working definition of “inappropriately housed.” Instead, Ministry staff later decided to contact hospitals directly as part of the project, to identify eligible individuals in hospital.
Lack of information
287 One of the recommendations from Nowhere to Turn specifically addressed the need to gain better insight into the hospitalization of individuals with developmental disabilities by regularly obtaining information from hospitals across the province.[68] In response to the recommendation, the then-Ministry of Community and Social Services said that privacy considerations prevented the collection of information about individuals in hospital without their consent.
288 During the joint Dual Diagnosis Alternate Level of Care Project, the two ministries attempted to navigate this complication. For instance, Ontario Health and developmental services staff contacted hospitals directly to inquire about eligible individuals. However, they still encountered some roadblocks related to patient confidentiality.
289 During this investigation, MCCSS officials told us that the developmental services reform envisioned in Journey to Belonging would include “some kind” of information technology changes once government policy decisions are made. MCCSS staff said any ideas to improve the data quality have been put on hold while developmental services reform is ongoing and because of “resource constraints.” They said developmental services “has not been one of the early programs for us to be supporting in terms of changing the data platform,” and there is no timeframe for the work to be done.
Connecting the data: The case for an integrated data system
290 Senior officials with both ministries consistently agreed in our interviews that better data is required to understand and support this patient population more effectively, and to inform funding decisions on services and approaches. A senior MOH staff member working on the Dual Diagnosis Alternate Level of Care Project remarked that “it’ll just be a revolving door” if the ministries do not gather reliable data to support the systemic work to prevent people from becoming alternate level of care in hospital. They observed that the ministries need to do a better job to define the data needed, and then collect it.
291 The MOH has prepared a hospital engagement plan and has surveyed hospital dual diagnosis programs to gather information about the individuals who remain in hospital due to a lack of community discharge option. The MOH has also engaged the Institute for Clinical Evaluative Sciences and the Centre for Addiction and Mental Health to examine trends in long-stay patients in hospital mental health beds who have developmental disabilities. The study is focusing on long-stay hospitalizations rather than alternate level of care, because they recognize that not everyone is formally designated.
292 The findings stated that, as of September 2023, there were 555 patients with developmental disabilities who had remained in a mental health bed for more than a year. This represented 28% of all long-stay mental health patients.[69] However, we know that individuals with developmental disabilities can be housed in hospital units apart from mental health units, so the number may be much higher.
293 The information gathered through this study will be valuable for planning purposes, but ongoing collection of more precise and sufficient data is needed to enable the ministries to monitor trends and better plan for appropriate developmental and health services. Reliable data on hospitalization trends will also be helpful to gauge whether efforts to prevent inappropriate hospitalizations are effective or need to be adjusted.
294 On an individual level, a more reliable and accurate reporting system between hospitals and DSO is needed so that people are not overlooked and can be prioritized and connected to needed services based on their actual circumstances. A senior DSO official explained that communication with them is key when someone remains in hospital awaiting appropriate services.
295 It is imperative that the ministries jointly develop a method for gathering and sharing accurate and comprehensive information about alternate level of care and long-stay patients with developmental disabilities. This will assist with individual and system planning, with the aim of reversing the trend of hospitals acting as default housing for individuals with developmental disabilities and complex needs.
296 Provided that modifications to their respective information systems and information sharing are feasible, given the current system limitations and the different purposes for which the systems exist, the ministries should consider developing a new, integrated information system model designed specifically to capture information about patients with developmental disabilities. They should also explore mechanisms to address confidentiality concerns that could hamper attempts to share information between the developmental services and hospital sectors. They should engage with hospitals and developmental services and the Information and Privacy Commissioner to discuss confidentiality barriers, and consider a legislative response if necessary.
Recommendation 15
The Ministry of Children, Community and Social Services and the Ministry of Health should work together to develop an effective method of collecting and sharing accurate and timely information about alternate level of care and long-stay patients with developmental disabilities, to assist with planning.
Recommendation 16
The Ministry of Children, Community and Social Services and the Ministry of Health should consult with the Information and Privacy Commissioner to explore mechanisms to address patient confidentiality concerns that hamper attempts to share necessary information between the developmental services and hospital sectors.
Staffing challenges
297 One of the pillars of the government’s Journey to Belonging vision for developmental services reform is growing and stabilizing a skilled, diverse and professional developmental services workforce.
298 We repeatedly heard from MCCSS and developmental service agency officials that staffing shortages and the difficulty of recruiting and retaining qualified staff are obstacles to long-stay patients transitioning to homes with suitable support in the community. In Sean’s case, the service agency that tried to find 3:1 staffing support for him in a rural location attended job fairs, held its own job fairs, contacted colleges and developmental support worker programs to offer placements, tried new online hiring platforms and even reduced their hiring eligibility and experience requirements. Despite all these efforts, the agency was unable to recruit sufficient staff.
299 In 2018, Queen’s University published a Ministry-funded evaluation of Ontario’s 2008 10-year Developmental Services Human Resources Strategy.[70] Although it noted some positive trends, the report found that recruitment remained one of the most pressing issues reported by service agencies in a tight labour market. KPMG’s 2020 review of developmental services observed that the Ministry had “no unified workforce strategy” to support and grow the workforce.[71]
300 In 2023, Ontario Agencies Supporting Individuals with Special Needs, an organization that represents more than 190 Ontario developmental service agencies, called for a comprehensive sector staffing strategy and related funding.[72] They stated that this would be “crucial to realizing the vision set out in Journey to Belonging.” More recently, a December 2024 paper by Community Living Ontario and the Ontario Agencies Supporting Individuals with Special Needs stated that service agencies that rely on developmental support workers are facing “immediate and ongoing workforce shortages.”
301 Service agencies told us there are not enough developmental service worker graduates to keep up with demand for qualified support staff. Some agencies have started hiring underqualified people and conducting additional training on the job. One developmental services professional said service agencies often lack the resources to pay workers appropriately and to provide the extensive training necessary to support individuals with higher needs. A larger service agency told us they have been able to build some capacity internally by providing staff with behavioural competency training, but this requires resources that not all agencies have. They suggested that if the Ministry invested in this type of training, it could help build staff capacity and confidence to support individuals with complex needs.
302 As part of the Dual Diagnosis Alternate Level of Care Project, the MCCSS worked with community partners to develop a series of micro-credential courses aimed at increasing staff capacity to support adults with dual diagnosis transitioning from hospital alternate level of care beds. However, just under 200 staff had participated or enrolled in the courses as of January 2025, in a workforce of over 23,000 full-time staff.
303 Service agencies told us the COVID-19 pandemic exacerbated existing staffing shortages and recruitment challenges, as many developmental service professionals left for other careers. One agency told us they had two homes sitting empty because of staffing shortages and 32 full-time vacancies. One regional Ministry official said:
I have seen a very big slowdown in the last few years in terms of ability to have enough staff even to maintain service continuity. The pandemic really took a toll. People in the sector left… 20-, 30-year employees left. They were just burned out. They were done.
304 MCCSS has taken some additional steps, in partnership with the Provincial Network on Developmental Services, to address recruitment challenges in the sector. For instance, a Ministry document from March 2023[73] refers to three new initiatives to support the developmental services workforce, including a recruitment-focused marketing campaign to promote the sector as a career, modernized core competencies for developmental services workers to provide more individualized, person-directed supports, and a leadership training program. A senior Ministry official also told us that future policy work on Journey to Belonging would involve working with the sector on workforce strategies, based on government decision-making over a trajectory of 8-10 years. In the meantime, individual agencies and community planning tables have been working to address local recruitment and retention issues.
305 Until 2019, the Ministry of Children, Community and Social Services collected detailed staffing data from service agencies through annual reporting processes. However, when the government implemented a new system (Transfer Payment Ontario) in 2020, the staffing data was “drastically scaled back” to reduce administrative burden on transfer payment agencies, including developmental service agencies. According to internal documents, the Ministry then lacked the “comprehensive and detailed workforce data essential to plan for the sector’s workforce and support program and policy decisions.” It was also unable to “confirm, predict, or address sector workforce pressures or trends” for Ministry-funded agencies.[74]
306 In 2024, the MCCSS began developing a workforce data strategy to try to address the knowledge gap. A Ministry official told us the timeline for data improvement is the end of fiscal year 2025-2026.
307 Despite recent efforts, challenges in recruitment and retention of qualified staff continue to frustrate attempts to help long-stay patients transition to the community. They also undermine the government’s Journey to Belonging goals of choice and inclusion. This problem has plagued the sector for many years and has intensified as demand for supportive community living increases. There are no quick fixes. However, I am recommending that the Ministry of Children, Community and Social Services make further efforts to identify and study the root causes of staff shortages in the developmental services sector and develop and implement meaningful and effective recruitment and retention initiatives and strategies. In furtherance of this goal, the Ministry should regularly collect and monitor relevant recruitment and retention information. The Ministry should also study and report on the results of its efforts.
Recommendation 17
The Ministry of Children, Community and Social Services should identify and study the root causes of staff shortages in the developmental services sector, including through regular collection and monitoring of relevant recruitment and retention information.
Recommendation 18
The Ministry of Children, Community and Social Services should work with the sector to develop and implement meaningful and effective recruitment and retention initiatives and strategies for the developmental services sector, and review and report on the resulting outcomes to my Office semi-annually.
Lack of supports in French
308 For the most vulnerable, including those with developmental disabilities who are inappropriately hospitalized, receiving services in their own language can significantly impact their health outcomes. The 2021-2022 Annual Report of the French Language Services Commissioner described a study published in the Canadian Medical Association Journal by 11 researchers on language concordance between patients and their physicians. The study found that Francophones who received care in their own language were “significantly less likely to have a harmful hospital admission or die in hospital [...] than Francophones who received language-discordant care. Furthermore, the average length of stay in hospital was 7% shorter for Francophones who received language-concordant care.”[75]
309 During this investigation, we heard from Francophones who described the negative consequences for people with developmental disabilities who could not access supports in hospital in French, and the added challenges they face in finding services in their language in the community. Luc’s situation illustrates the detrimental effects that can accompany a lack of developmental and health care services in French. Repeated failure to meet Luc’s communication needs intensified his struggles in hospital and the lack of French services in the community has prolonged his stay.
Limited French capacity
310 Service agencies within the developmental services sector that require bilingual or Francophone staff face major recruitment challenges. One MCCSS regional staff member who worked closely with agencies to support Luc acknowledged that recruitment for Francophone staff is significantly harder.
311 In Luc’s case, finding an agency with adequate French-speaking staff to support him while he is in hospital presents substantial difficulty. The lack of bilingual staff in developmental service agencies has also been a key obstacle to Luc’s transition out of hospital. Developmental service agencies considering supporting Luc, including those at both French- and English-language planning tables, lacked confidence that they could find enough staff to support him at the 3:1 ratio he requires. The need to ensure sufficient Francophone or bilingual staff compounds the situation.
312 The service agency that was originally planning for Luc was the only Ministry-funded service agency in the province providing services exclusively in French. Two other homes in the area that could provide bilingual or French services either did not have capacity or could not serve individuals with complex needs.
313 Another agency with French-speaking staff has stepped forward that may potentially be able to develop a transition plan for him, but it is in very early stages. At the time of writing this report, Luc remains in hospital.
314 Luc’s situation is not unique. Service agencies we spoke with described other cases of Francophones with developmental disabilities in hospital having to accept service from agencies that could not serve them in French. They said some patients had to leave their region to find supportive living in the community. One developmental services official remarked:
[I]n order to leave the hospital, although their family and their community is here, they’ve had to leave, out of region, in order to get a home. And that’s not fair either…
315 Ministry staff told us that, as part of their oversight role, they work with agencies on quality improvement plans, including French language plans, to develop their French service capacity. However, they also acknowledged that these plans take several years to implement because agencies cannot create new positions or build capacity without additional funding and otherwise must wait for unilingual staff to leave before they can recruit bilingual or French-speaking staff.
316 As part of the Journey to Belonging planning, the MCCSS engaged with Francophone groups and stakeholders and sought feedback on various topics, including supportive housing and complex needs. However, Ministry officials told us they are still in the planning phase in terms of how to address the French language service gaps identified through the feedback.
317 MCCSS officials told us the East Region is home to 43% of Ontario’s Francophone population. They said the Ministry has made investments to try to build French language service capacity over the years in the region. However, one of the challenges to increasing capacity for French-speaking individuals is that the Multi-Year Supportive Living Planning has no targeted investments specific to the Francophone population, and the funding reflects individual prioritization. Ministry staff also said that, although DSO’s data system can record information about an individual’s language preference, there are limitations on the system’s reporting capability that make it difficult for MCCSS regional offices to monitor how many people on the supportive living registry require services in French.
318 The MCCSS should develop a more efficient method of tracking the number of individuals registered with DSO who require supportive living services in French. I have already recommended that the MOH and MCCSS work together to develop an effective method of collecting and sharing necessary planning information about alternate level of care and long-stay patients with developmental disabilities. As part of that collaborative effort, the Ministries should work with system partners to develop methods of tracking the number of long-stay French-speaking patients with developmental disabilities in hospital.
319 The MCCSS should use the information collected about French language service needs to develop and implement initiatives and strategies to increase the availability of French-speaking staff in the developmental services sector and to inform broader system planning.
Recommendation 19
The Ministry of Children, Community and Social Services should develop a more efficient method of tracking the number of individuals registered with Developmental Services Ontario who require supportive living services in French.
Recommendation 20
The Ministry of Children, Community and Social Services and Ministry of Health should work with system partners to develop methods of tracking the number of French-speaking patients with developmental disabilities in hospital and the length of their hospitalization.
Recommendation 21
The Ministry of Children, Community and Social Services should use the information collected about French language service needs to develop and implement initiatives and strategies to increase the availability of French-speaking staff in the developmental services sector and to inform broader system planning.
Clinical supports for Francophones
320 In addition to challenges in finding developmental support workers who speak French, there are also challenges in locating bilingual clinical specialists, such as psychologists and psychiatrists, who can support Francophones with developmental disabilities.
321 The French Language Specialized Services Resource (“La Ressource”) is embedded in the Community Network of Specialized Care. La Ressource supports initiatives to improve provincewide access to specialized clinical services in French. It helps service agencies and professionals connect individuals who have developmental disabilities and mental health, behavioural, or other complex needs to clinical resources in French. However, such resources remain limited.
322 The MOH is aware of French language service access issues. Officials told us they work to improve access, including through technology, such as tele-mental health. They noted that there have been investments mental health supports in French through the Ministry’s “Roadmap to Wellness,” but these are not specific to individuals with developmental disabilities.
323 The MOH and MCCSS should work together, through the joint forum I have recommended they create, to develop and implement initiatives and strategies to increase the availability of clinical supports to serve French-speaking individuals with developmental disabilities and assist their successful transition from hospital to the community.
Recommendation 22
The Ministry of Health and the Ministry of Children, Community and Social Services should work together to identify and develop initiatives and strategies to increase the availability of clinical supports to serve French-speaking individuals with developmental disabilities and assist their successful transition from hospital to the community.
Opinion
324 Uniquely vulnerable members of our society are entitled to have their rights respected and to live with dignity in humane, compassionate conditions. The stories of Jordan, Jack, Luc, Noah, Sean, Kevin and Anne – along with many others like them – are marked by deprivation and decline, resulting from prolonged and inappropriate hospitalization.
325 The experiences of the seven people featured in this report fall deplorably short of the purposes reflected in the Services and Supports to Promote the Social Inclusion of Persons with Developmental Disabilities Act and the goals of the MCCSS’ Journey to Belonging – goals of empowerment, independence, and person-directed, equitable, and sustainable supports.
326 Individuals with developmental disabilities and complex needs continue to find themselves suffering for unnecessarily long periods in Ontario hospitals and psychiatric facilities at a concerning rate. Hospitals have become housing by default for many of those with the most complex needs within a system that is well beyond capacity to provide the intensive supports and services they require in the community. This is simply unacceptable.
327 Stranded in institutional environments that were not designed to meet their needs, some of these individuals become confused, frustrated, and dysregulated, leading to the routine application of chemical and physical restraints. Despite the efforts of health care and social services staff, many face deplorable and unacceptable conditions. During extended hospitalization, it is common for them to regress and lose hard-won skills and abilities. The longer the period of hospitalization, the harder it is to find a service agency capable and willing to help them transition to the community. The cost associated with supportive living in the community also increases with prolonged hospitalization.
328 It is disheartening to see how little the situation has changed since I published Nowhere to Turn in August 2016. During this investigation, we learned that in 2017 and 2018, the Ministry of Children, Community and Social Services had actively prepared a strategy, collaborated on a supportive housing framework, and was planning initiatives to address the issue of individuals with developmental disabilities inappropriately housed in settings such as hospitals. However, these plans stalled and were never revived.
329 The chronic shortage of suitable supports and supportive living accommodations, particularly for those with complex needs, shows no signs of abating. There is limited progress in proactive long-range system planning, and instead, only short-lived, ad hoc projects and initiatives. Although the joint Ministry Dual Diagnosis Alternate Level of Care Project addressed an acute need for a brief time, it only dealt with cases one by one, and left the system in the same unacceptable state as where it started.
330 For years, successive researchers have emphasized the need for better collaboration, systemic planning, coordination and integrated services across the health care and developmental services sectors. But the two systems remain divided and siloed.
331 Given the disturbing increase in individuals with developmental disabilities and complex needs who require supports, the situation will only worsen over time. The government developed aspirational goals in Journey to Belonging with a timeline of 8-10 years – but they will never become a reality unless real and urgent changes are made.
332 The Ministry of Children, Community and Social Services is charged with oversight of the developmental services sector, which includes provision of supports and services to “vulnerable citizens.” However, during this investigation, several Ministry officials emphasized that developmental services are not an entitlement program. Others seemed to accept that the problem of limited resources to meet the needs of this population is insurmountable. I am concerned that these attitudes reflect an ingrained sense of defeat, which if it continues, threatens to breed complacency and inaction. Given its lead in the sector, the MCCSS should be a champion for change. It should proactively and energetically seek solutions to the current situation, in which hospitals frequently serve as default housing for individuals with developmental disabilities in crisis.
333 For years, the Ministry has failed to effectively address situations involving long-stay patients with developmental disabilities. It has not planned proactively to address the lack of adequate supportive living options in the community, including for those requiring supports and services in French. It has also failed to ensure that it has accurate information necessary for system planning.
334 The Ministry of Health oversees Ontario’s health care system. It is well aware of the difficulties faced by people with developmental disabilities who are confined inappropriately in hospitals without adequate developmental supports – as well as the strain such extended hospitalizations create for health care staff, and the resulting impact on access to acute care beds.
335 Together, the Ministry of Children, Community and Social Services and the Ministry of Health have failed to work together effectively to share information, develop communication practices, and engage in system planning to address the issue of inappropriate hospitalization of individuals with developmental disabilities. They have also failed to construct effective pathways or integrated supports for patients to transition to appropriately supported settings in the community, reducing the impacts of hospital stays and likelihood of readmission. Accordingly, it is my opinion that the conduct of both ministries is unreasonable and wrong under the Ombudsman Act.
336 The recommendations I have made are intended to guide both ministries and assist them in planning, developing strategy, and implementing projects and initiatives aimed at reducing the frequency of individuals with developmental disabilities languishing in Ontario’s hospitals. The current situation has immense human costs to the individuals themselves, as well as their families. It also creates an unsustainable burden on the health care system, increasing the challenges faced by those working in the health care and developmental sectors, and restricting access to scarce acute care beds. I am hopeful that by shining light on seven individuals whose lives were suspended while they were trapped in hospital and left to deteriorate, this report will lead to long overdue reform and concrete and lasting systemic improvement.
337 I urge both ministries to collaborate closely and work together in their review and response to this report. I will carefully monitor their progress in implementing my recommendations.
Recommendation 23
The Ministry of Children, Community and Social Services and Ministry of Health should jointly report to my Office in six months’ time on their joint progress in implementing my Recommendations 1, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 20 and 22, and at six-month intervals thereafter, until I am satisfied that adequate steps have been taken to address them.
Recommendation 24
The Ministry of Children, Community and Social Services should report to my Office in six months’ time on their progress in implementing my Recommendations 2, 3, 4, 17, 18, 19 and 21, and at six-month intervals thereafter, until I am satisfied that adequate steps have been taken to address them.
Recommendations
Given the results of this investigation, I am making the following recommendations:
Recommendation 1
The Ministry of Children, Community and Social Services and the Ministry of Health should immediately establish a standing joint forum to engage in proactive system planning for individuals with developmental disabilities and complex needs. The forum should engage with any developmental services and health partners necessary for effective planning. The joint forum should commence its work no later than six months from the issuance of my report and should work collaboratively to address the barriers facing alternate level of care and long-stay patients with developmental disabilities and complex needs in transitioning to appropriate supportive housing in the community. The joint forum should report to the Deputy Ministers of each ministry and provide a semi-annual progress update to my Office.
Recommendation 2
The Ministry of Children, Community and Social Services should include capital planning and funding as part of proactive developmental services system planning, in order to develop adequate and appropriate community infrastructure to accommodate the needs of individuals with developmental disabilities, including those with more complex needs.
Recommendation 3
The Ministry of Children, Community and Social Services should include financial forecasting of service agency costs and vacancy management as part of its proactive system planning.
Recommendation 4
The Ministry of Children, Community and Social Services should develop a transparent process for negotiating budgets to meet increased individual and service agency needs as part of its proactive system planning. This process should include clear eligibility and decision-making criteria that are provided to my Office and communicated across the sector.
Recommendation 5
The Ministry of Children, Community and Social Services and the Ministry of Health should work together, through the joint forum referred to in Recommendation 1, to identify and implement an integrated approach and appropriate care framework for delivering services and supports across the developmental services and health sectors to prevent unnecessary hospitalizations and support patients with developmental disabilities with complex needs in hospital, during transition, and post-discharge in the community.
Recommendation 6
The Ministry of Children, Community and Social Services and the Ministry of Health’s joint forum, referred to in Recommendation 1, should work towards ensuring patients have access to necessary developmental supports while in hospital and clinical supports during and after transition to the community.
Recommendation 7
The Ministry of Children, Community and Social Services and the Ministry of Health should, as a priority, work together to update, publish, and implement the Joint Policy Guideline for the Provision of Community Mental Health and Developmental Services for Adults with a Dual Diagnosis.
Recommendation 8
The Ministry of Children, Community and Social Services and the Ministry of Health should extend the application of the Joint Policy Guideline for the Provision of Community Mental Health and Developmental Services for Adults with a Dual Diagnosis to individuals with developmental disabilities and complex needs who do not have a mental health diagnosis.
Recommendation 9
The Ministry of Children, Community and Social Services and the Ministry of Health should publish and annually update meaningful information on their websites about waitlist numbers for Ministry-funded supportive living, potential wait times, the number of annual vacancies that arise, and the number of people served by each funded supportive living type.
Recommendation 10
The Ministry of Children, Community and Social Services and the Ministry of Health, through the joint forum referred to in Recommendation 1, should work together to develop and implement an ongoing education and training program for the health sector, focused on providing information about developmental services and dual diagnosis resources, programs and processes, to assist with discharge planning for patients with developmental disabilities.
Recommendation 11
The Ministry of Children, Community and Social Services and the Ministry of Health, through the joint forum referred to in Recommendation 1, should work together to develop and implement a joint protocol governing communication concerning patients with developmental disabilities, including around notification of Developmental Services Ontario when such patients are admitted and become long-stay or alternate level of care, and to support transition/discharge planning.
Recommendation 12
The Ministry of Children, Community and Social Services and the Ministry of Health’s joint protocol, referred to in Recommendation 11, should clearly set out the respective roles, responsibilities, and expectations for developmental services and health partners, and provide for participation of relevant hospital staff at planning table discussions.
Recommendation 13
The Ministry of Health and the Ministry of Children, Community and Social Services should encourage increased communication between health and developmental services sector professionals concerning issues of mutual interest through an appropriate, structured mechanism.
Recommendation 14
The Ministry of Children, Community and Social Services and the Ministry of Health’s joint protocol, referred to in Recommendation 11, should include specific provisions relating to the sharing of patient information to facilitate transition planning for individuals with developmental disabilities.
Recommendation 15
The Ministry of Children, Community and Social Services and the Ministry of Health should work together to develop an effective method of collecting and sharing accurate and timely information about alternate level of care and long-stay patients with developmental disabilities, to assist with planning.
Recommendation 16
The Ministry of Children, Community and Social Services and the Ministry of Health should consult with the Information and Privacy Commissioner to explore mechanisms to address patient confidentiality concerns that hamper attempts to share necessary information between the developmental services and hospital sectors.
Recommendation 17
The Ministry of Children, Community and Social Services should identify and study the root causes of staff shortages in the developmental services sector, including through regular collection and monitoring of relevant recruitment and retention information.
Recommendation 18
The Ministry of Children, Community and Social Services should work with the sector to develop and implement meaningful and effective recruitment and retention initiatives and strategies for the developmental services sector, and review and report on the resulting outcomes to my Office semi-annually.
Recommendation 19
The Ministry of Children, Community and Social Services should develop a more efficient method of tracking the number of individuals registered with Developmental Services Ontario who require supportive living services in French.
Recommendation 20
The Ministry of Children, Community and Social Services and Ministry of Health should work with system partners to develop methods of tracking the number of French-speaking patients with developmental disabilities in hospital and the length of their hospitalization.
Recommendation 21
The Ministry of Children, Community and Social Services should use the information collected about French language service needs to develop and implement initiatives and strategies to increase the availability of French-speaking staff in the developmental services sector and to inform broader system planning.
Recommendation 22
The Ministry of Health and the Ministry of Children, Community and Social Services should work together to identify and develop initiatives and strategies to increase the availability of clinical supports to serve French-speaking individuals with developmental disabilities and assist their successful transition from hospital to the community.
Recommendation 23
The Ministry of Children, Community and Social Services and Ministry of Health should jointly report to my Office in six months’ time on their joint progress in implementing my Recommendations 1, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 20 and 22, and at six-month intervals thereafter, until I am satisfied that adequate steps have been taken to address them.
Recommendation 24
The Ministry of Children, Community and Social Services should report to my Office in six months’ time on their progress in implementing my Recommendations 2, 3, 4, 17, 18, 19 and 21, and at six-month intervals thereafter, until I am satisfied that adequate steps have been taken to address them.
Response
338 I provided the Ministry of Children, Community and Social Services and the Ministry of Health with the opportunity to review and respond to my preliminary findings, opinion, and recommendations. The Ministries’ comments and input were carefully considered in the preparation of this final report.
339 In their joint response, the Ministries accepted all of my recommendations and confirmed their commitment to working with my office and system partners to improve outcomes for individuals with developmental disabilities and complex needs. The Ministries acknowledged the need for a co-ordinated and sustained approach to providing care and supports in the appropriate settings.
340 In addition to identifying the need for integrated planning and improved cross-sector collaboration, the Ministries committed to improve data sharing and communication. They outlined steps they have taken to date to support transition of individuals out of hospital, including through the Dual Diagnosis Alternate Level of Care Project. They also confirmed their continued vision for a more person-centred system to better address individual needs and goals. In their response, the Ministries recognize that improvements require a “multi-sectoral, coordinated, and sustained approach” to ensure the right supports are provided to individuals in the right place – an approach that will require a significant shift from the status quo in many ways.
341 I am encouraged by the Ministries’ commitment to work together to prevent the types of inappropriate, dehumanizing, and lengthy hospitalizations described in this report. I urge the Ministries to embrace and act swiftly on my recommendations to make their services and planning more proactive and integrated. In the face of a complex system, these changes will necessitate sustained commitment from both Ministries to enable individuals with developmental disabilities to live safe and fulfilling lives in the community.
342 I will closely monitor the Ministries’ progress in implementing my recommendations, and look forward to their ongoing cooperation with my Office.
__________________
Paul Dubé
Ombudsman of Ontario
[1] The names used in this report have been changed to protect the confidentiality of the individuals who shared their stories with us.
[2] Ombudsman Act (Re), 1970 CanLII 798 (AB KB), online.
[3] Institute for Clinical Evaluative Sciences and the Centre for Addiction and Mental Health, Health Care Access Research and Developmental Disabilities program: “Long-Stay Patients in Ontario Mental Health Beds with Developmental Disabilities”, October 2024 “H-CARDD snapshot”, online.
[4] More detailed information regarding the history of developmental services in Ontario can be found in: Ombudsman Ontario Nowhere to Turn, 2016, online.
[5] Ontario Backgrounder (now archived), “Closing Institutions for People with a Developmental Disability”, March 31, 2009, online.
[6] Developmental Services Act, R.S.O. 1990, c D.11 (repealed on July 1, 2011).
[7] Services and Supports to Promote the Social Inclusion of Persons with Developmental Disabilities Act, 2008, S.O. 2008, c.14.
[8] Ministry of Children, Community and Social Services’ vision for developmental services, online.
[9] Ombudsman Ontario Nowhere to Turn, 2016, online.
[10] Your Health: A Plan for Connected and Convenient Care, ontario.ca, online.
[11] The Ontario Disability Support Program provides income support for basic needs and shelter for eligible adults with disabilities. Funding varies depending on individual income and circumstances. Effective July 1, 2025, a single person can receive up to $1,408 per month for basic needs and shelter, online.
[12] Individuals with developmental disabilities may be eligible for $5,500 to $44,275 per year to help pay for needed services and supports, such as hiring a direct support professional, accessing respite, and participating in community programs, online.
[13] Ontario Health website, online.
[14] Connecting Care Act, 2019, S.O. 2019, c. 5, Sched. 1, s. 6.
[15] Ontario Health Alternate Level of Care (ALC) Reference Manual April 1, 2021 Version 3, online.
[16] MCCSS Adult Developmental Services. Minister Briefing – Foundational Information: April 12, 2023.
[17] Financial Accountability Office of Ontario: Ministry of Children, Community and Social Services: Spending Plan Review, 2024; p. 20, online.
[18] 2016 Annual Report Office of the Ontario Auditor General; 3.07 Housing and Supportive Services for People with Mental Health Issues (Community-Based), online.
[19] Addictions and Mental Health Ontario, Policy Recommendations for Mental Health and Addictions Supportive Housing in Ontario, February 2024, online.
[20] Addictions and Mental Health Ontario: Ganesan, K., Matte, A., Williams, AR., Wilkie J., Chan., C., O’Connor, K. (2025). Unlocking Solutions: Understanding and Addressing Ontario’s Mental Health and Addictions Supportive Housing Needs, online.
[21] DD ALC Client Proposal Form, October 27, 2021 and DD ALC MOH and MCCSS Master List November 2021.
[22] Program Note. Community and Social Services – DS Residential Services (Adults), October 9, 2018.
[23] MCCSS Developmental Services Reform Foundational Papers, Residential Services and Supports, July 23, 2019.
[24] Addictions and Mental Health Ontario: Policy Recommendations for Mental Health & Addictions Supportive Housing in Ontario, February 2024, online.
[25] MCCSS Adult Developmental Services. Minister Briefing – Foundational Information. April 2023.
[26] 2022-23 MHA My Proposal Template; September 9, 2021; OO Overview DD ALC PowerPoint presentation May 3, 2023.
[27] MCCSS April 12, 2023 Developmental Services Foundational Deck Minister Briefing.
[28] Ombudsman Ontario Nowhere to Turn, 2016, p. 87 par. 291, 292, online.
[29] Ombudsman Ontario Nowhere to Turn, 2016, p. 120, par. 393 Recommendation 54, online.
[30] Financial Accountability Office of Ontario: Ministry of Children, Community and Social Services Spending Plan Review, online.
[31] Dale Butterill MSW, MPA; Elizabeth Lin, PhD; Janet Durbin, PhD; Yona Lunsky, PhD; Karen Urbanoski, PhD (Candidate); and Heather Soberman, MA: From Hospital to Home: The Transitioning of Alternate Level of Care and Long-stay Mental Health Clients, Centre for Addiction and Mental Health, September 2009.
[32] Provincial Review of Dual Diagnosis Programs: Final Report, October 5, 2012, KPMG.
[33] Ontario Developmental Services Housing Task Force – Final Report 2018, “Generating Ideas and Enabling Action: Addressing the Housing Crisis Confronting Ontario Adults with Developmental Disabilities”, online.
[34] Lin E, Balogh RS, Durbin A, Holder L, Gupta N, Volpe T, Isaacs BJ, Weiss JA, Lunsky Y, Addressing Gaps in the Health Care Services Used by Adults with Developmental Disabilities in Ontario, Toronto, ON: ICES; 2019.
[35] Centre for Addiction and Mental Health, Housing and Mental Health Policy Framework; February 2022, online.
[36] Selick, A., Morris, S., Volpe, T. & Lunsky, Y. (2023), Supporting alternate level of care (ALC) patients with a dual diagnosis to transition from hospital to home: Practice guidance, Toronto, ON: Centre for Addiction and Mental Health, online.
[37] Ombudsman Ontario Nowhere to Turn, 2016, p. 17, para. 58, online.
[38] Ontario Supportive Housing Policy Framework, March 2017, online.
[39] MCCSS Housing and Supports for Adults with a Developmental Disability DS Housing Strategy April 17 & 18, 2018.
[40] Memorandum to Ministry Management Committee, Subject: MCCSS Expenditure Management Strategy, From Assistant Deputy Minister; August 22, 2018.
[41] Ministry of Children, Community and Social Services Minister’s Information Note (September 2018).
[42] Ontario Developmental Services Housing Task Force – Final Report 2018, “Generating Ideas and Enabling Action: Addressing the Housing Crisis Confronting Ontario Adults with Developmental Disabilities”, online.
[43] MCCSS Developmental Services Reform Foundational Papers: Residential Services and Supports (July 2019).
[44] Developmental Services: Opportunities for a Sustainable Delivery Model (Draft) KPMG, February 6, 2020.
[45] MCCSS Developmental Services Housing Deck, Appendix E – August 17, 2022.
[46] MCCSS DS Housing Initiatives Review – Director's Discussion (PowerPoint), August 18, 2022.
[47] Ministry of Children, Community and Social Services, Information Note (November 19, 2020).
[48] 2021/22 Multi-Year Residential Planning Strategy (PowerPoint); Regional Directors & Community Program Managers: March 5, 2021, Draft Material for Discussion.
[49] Shortt (Re), 2020 ONCA 651 (CanLII), online.
[50] Dual Diagnosis Alternate Level of Care - Action Plan (PowerPoint), February 2023.
[51] 2023-24 Strategic Decisions Template: Social Services Infrastructure Strategy Request, MCCSS.
[52] MCCSS Developmental Services Reform Foundational Papers: Residential Services and Supports July 2019.
[53] Cross-Sector Complex Care Model: Evaluation Report: York Region Pilot. April 24, 2017, Cathexis Consulting Inc.
[54] Lin E, Balogh RS, Durbin A, Holder L, Gupta N, Volpe T, Isaacs BJ, Weiss JA, Lunsky Y, Addressing Gaps in the Health Care Services Used by Adults with Developmental Disabilities in Ontario, Toronto, ON: ICES; 2019. ISBN: 978-1-926850-85-6, online.
[55] Selick, A., Morris, S., Volpe, T. & Lunsky, Y. (2023), Supporting alternate level of care (ALC) patients with a dual diagnosis to transition from hospital to home: Practice Guidance, Toronto, ON: Centre for Addiction and Mental Health, online.
[56] Dual Diagnosis Transitional Rehabilitation Housing Program (DD TRHP) - This program supports individuals with developmental disabilities and/or a dual diagnosis who are on a forensic ward under an Ontario Review Board (ORB) disposition. These individuals have been deemed not criminally responsible, or unfit to stand trial, as a result of conflict with the law. The Community Treatment Home is a transitional program to teach, support, and develop daily living skills to allow these individuals to return to the community as participating citizens.
[57] 2022/23 - 2024/25 Multi-Year Residential Planning (MYRP) for DS Planning Partners.
[58] February 6, 2020 KPMG Report Draft; “Developmental Services: Opportunities for a Sustainable Delivery Model”.
[59] MCCSS Developmental Services Foundation Briefing January 2021.
[60] MCCSS Health Access Barriers (DS Reform) PowerPoint presentation: September 28, 2021.
[61] Ministry of Health and Long Term Care and Ministry of Community and Social Services, Joint Policy Guideline for the Provision of Community Mental Health and Developmental Services for Adults with a Dual Diagnosis, December 2008, online.
[62] Provincial Review of Dual Diagnosis Programs: Final Report, October 5, 2012, KPMG.
[63] Improving Linkages Between the Health and Developmental Services Sectors, Manager’s PCC, November 13, 2018.
[64] Dual Diagnosis Framework: Proposed Next Steps, Community Supports Policy Branch, MCCSS, and Mental Health and Addictions Branch, MOHLTC November 2018.
[65] Dual Diagnosis Framework, Proposed Next Steps, Community Supports Policy Branch, MCCSS and Mental Health and Addictions Branch, MOHLTC November 2018 PowerPoint Presentation.
[66] Selick, A., Morris, S., Volpe, T. & Lunsky, Y. (2023), Supporting alternate level of care (ALC) patients with a dual diagnosis to transition from hospital to home: Practice guidance, Toronto, ON: Centre for Addiction and Mental Health.
[67] Provincial Network on Developmental Services: A Call to Action for Fundamental Cross-Sectoral Change, Advancing access, equity, and improved health outcomes for persons living with intellectual and developmental disabilities, a position paper from the Health Strategy and Engagement Working Group September 2023, online.
[68] Ombudsman Ontario Nowhere to Turn, 2016, Recommendation 15, online.
[69] Health Care Access Research and Developmental Disabilities: Long-Stay Patients in Ontario Mental Health Beds with Developmental Disabilities, October 2024, online.
[70] Developmental Services Human Resource Strategy Evaluation Report: Summary Report, Assessing the impacts of the ten-year DSHR Strategy and informing continued efforts to advance workforce development and enhance HR practices in Ontario’s developmental services sector. Queen’s University Employment Relations Programs, Robert Hickey, Ph.D.
[71] KPMG: Developmental Services: Opportunities for a Sustainable Delivery Model (Draft), Ministry of Children, Community and Social Services, February 6, 2020.
[72] Ontario Agencies Supporting Individuals with Special Needs (OASIS), 2023 Advocacy Q&As, online.
[73] MCCSS Workforce Strategy Briefing Deck: Confidential Advice – updated November 28, 2023.
[74] MCCSS Workforce Data Strategy Status Update for ADMs January 17, 2025.
[75] Emily Seale, Michael Reaume, Ricardo Batista, Anan Bader Eddeen, Rhiannon Roberts, Emily Rhodes, Daniel I. McIsaac, Claire E. Kendall, Manish M. Sood, Denis Prud’homme and Peter Tanuseputro, CMAJ July 11, 2022 194 (26) E899-E908; DOI, online.